

May 2017, Volume 1 / Issue 1
AFPI Karnataka Quarterly Newsletter
President’s Letter
Dear Colleagues
I* gives me immense pleasure to present the inaugural edition of a quarterly electronic newsletter from Academy of Family Physicians of India (AFPI) Karnataka chapter. This newsletter seeks to foster communication and academic interaction among primary care providers.
Since the inception of AFPI Karnataka chapter on 1 st August 2015, we are striving to meet the academic needs of family physicians which is in line with our mission. We have con- ducted a number of conferences, CMEs and workshops catering to the needs of family physicians, DNB residents and hospital based family physicians. The need was felt to have a formal medium of communication containing information of interest to our members and to update them of AFPI activities. It is befitting to the efforts of our team that AFPI Karnataka chapter was adjudged the best state chapter in the recently conc*uded national conference at Kochi. It also gives me great pleasure to announce that *e have won the bid for hosting the next national conference of Family Medicine & Primary Care (FMPC) at Bangalore in the year 2019.
The newsletter also invites members to document reflections of their experiences in pri- mary care practice. I ap*reciate you taking the time to read our newsletter and look for- ward to your active contribution and valuable feed*ack. I am placing on record our sin- cere gratitude to the editorial team and wish them good luck in their endeavour to make this newsletter an interesting and enriching magazine for family physicians and others interested in family medicine.
Col (Dr.) Mohan Kubendra
AFPI Karnataka will be hosting the next National confer- ence of Family Medicine & primary care (FMPC) at Bangalore in the year 2019
President
Col (Dr.) Mohan Kubendra mohankubendra@gmail.com
Secretary
Dr. Bhaskara Puttarajanna drbhaskarap@gmail.com
Vice President
Dr. Ramakrishna Prasad dr.rk.prasad@gmail.com
Treasurer
Dr. Ravikumar Kulkarni ravikumarkulkarni@yahoo.com
Scientific Chair
Dr. Jaya Bajaj jayabajaj@gm*il.com
Editorial team
Dr. B. C. Rao badakere.rao@gmail.com
Dr. Roshni Jhan Ganguly roshnijhan@hotmail.com
Dr. Ramakrishna Prasad dr.rk.prasad@gmail.com
Inside this issue
|
AFPI News |
2 |
|||
|
Editorial Note |
Gleanings |
3 |
||
|
Case Reports |
5 |
|||
|
When we already have an active forum, why a newsletter? A forum, by its very nature is in*eractive |
Practice Experiences |
7 |
||
|
and is devoted to day to day issues. A newsletter, in contrast, is a more consolidated medium and |
11 |
|||
|
reaches out to all the members at the same time, thus makes one feel more a part of the larger fra- ternity of family medicine. We, the edito*ial team decided to keep this a completely electronic ver- sion, moreover an environment friendly one to capture events, updates, messages, articles and prac- tice experiences of family physicians. We have made a beginning and with your support, we will keep the AFPI flag unfurled for all times to come. |
Resident’s Corner Announcements |
12 |
||
AFPI NEWS
THE WAY FORWARD TO END TUBERCULOSIS


AFPI Karnataka in collaboration with the National Tuber- culosis Institute (NTI), organized a CME on ‘TB care in the private sector’ to commemorate World Tuberculosis Day on 24th March 2017. The event was a step forward to end this infectious disease. Through this event both the public and private sector discussed ways to streamline processes and make TB care more accessible, affordable, and collaborative*
The CME was presided by representatives of both AFPI (Dr. Mohan Kubendra and Dr. Soumya Vivek) and NTI (Dr. Prahlad Kumar, Dr. A Krishnamurthy, Dr. VK Chadha and Dr. Ravi Chandra). Dr. Raghunandan (State TB Officer) and Dr. Subramaniam (Senior Fam*ly Physi- cian) also participated.
ENT UPDATE
AFPI Karnataka conducted i*s first CME of this year in association with Bangalore Baptist Hospital on 2/4/17.
Family physicians commonly treat patients with *NT problems - spanning from simple p*aryngitis to the ‘confusing vertigo’. Along with history taking, practical skills are also important to adequately manage the pa- tient. Conducting hearing tests, proper use of the otoscope and performing effective maneuvers for diagnosing and relieving vertigo are some of these skills.
This CME focused on case based learning and hands on tra*ning. It was a joint effort of the family physicians of AFPI and the ENT specialists of Baptist hospital. The pro- gramme was packed with workshops and highly interac- tive sessions on key ENT topics like allergy, vertigo, emer- gencies in ENT, throat problems and hearing loss.
At the outset, Dr. Raghunandan, st*te TB officer commit- ted to cooperate and coordinate with primary care physi- cians. Dr. Prahlad Kumar recognized the important role of Family Physicians in putting an end to TB and empha- sized that family physicians are a great resource for TB care.
The scientific program started with Dr. Subramaniam talking about his experience in treating TB and the satis- faction that it has given him. He showed a study on the ‘Treatment outcomes of TB in his clinic’ and told us to become the nucleus of TB care delivery. Dr. Umashankar spoke on detection of TB (case finding and diagnosis) while Dr. Rav* Chandra highlighted newer advances on extra pulmonary TB. The updates in the treatment of TB were discussed by Dr. S K Tripathy. Dr. V K Chadha em- phasized enhanced and efficient systems available to en- sure proper TB care.
The CME concluded with a session on case scenarios and panel discussion conducted by Dr. Swapna Bhaskar and moderated by Dr. Ramakrishna Prasad. The panel discus- sion provided practical ways to navigate the complex health care ecosystem and resources available in both the private and public sectors. Contact details of the con- cerned personnel and organizations were provided and it was recommended that we develop a good rapport with our respective TB nodal officers for an effectively func* tioning system.
Dr. Srividhya Raghavendran along with Dr. Jaya Bajaj took the lead in organizing the event, along with the Bap- tist team of the family medicine residents. Family physi- cians - Drs. Mohammed Idris Shariff, Dhanya Ramdas, Archana Prabhakar, and Gowri Chintalapalli spoke on various topics. Dr. Soumya Vivek and Dr. Roshni Jhan Ganguly served as mentors. A special thanks to the ENT team (Dr. Badari Datta, Dr. Anita Thomas, Dr. Brinda Poojari, Dr. Manjula BV and Audiologist Ms. Sharanya) for their support. The hard work which organizers and mentors had put in to the event was reflected in the keen interest of the participants, and t*e enthusiasm they showed.
The Best Speaker award was bagged by Dr. Dhanya Ramdas (First Prize) and Dr. Archana Prabhakar (Second Prize).
2



First Quarterly CME by AFPI Karnataka iat Baptist Hospitak
REAL TIME LEARNING: EVERY SECOND FRIDAY NIGHT!
O* 24/3/17, Frida* night, AFPI Karnataka began a web based learnin* program on the Telegram forum. The des- ignated time was 2 hours from 8 to 10 pm. Dr. Pr*teek Reddy, a second year family medicine resident from St. Philomena’s Hospital, Bangalore, presented a case of UTI. Dr. Hasit Mehta, Urologist and Family Physician and Dr. B. C. Rao, Family Physician* moderated the dis- cussion. Most points related to the topic were covered. Around 17 members were online and took part in the dis- cussion. Few days later, Dr. Ratna Prasanna, Family Phy-
GLEANINGS
BIOSIMILARS
Biosimilars have been in the news lately. But what are they? Biosimilars are less expensive imitations of d*ugs known as biologicals such as rituximab, infliximab etc., which are used to treat a range of diseases including rheumatoid arthritis and many other conditions. Howev- er, they are not exact replicas.
Biologic drugs are made using living cells that are genet- ically modified. They are large and complex molecules, often many times the size of more common small- molecule drugs used in practice such as aspirin.
Making biosimilars is very challenging and involves coax-
sician, summarized the discussion and it was posted on our forum.
On 1*/4/17, there was a session on Hepatitis B. Modera- tors were Dr. B. C. Rao as Family Physician and Dr. Ra- makrishna Prasad in his capacity as Infectious Disease specialist. Several points of relevance to a practicing phy- sician were covered. Presentation and audience interac- tion was better as all of us were better prepared and ex- perienced in this novel method of learning. We hope to keep this program going on a biweekly basis.
ing living cells to produce an imitation molecule of the established biological. However, living cells are highly sensitive to their environments, and manufacturers have to create their own unique processes to make these cells do so.
However, the approval process for these drugs has its own challenges. Generics are approved based on match- ing chemical structure, but that doesn't work for biosimi- lars. Each new biosimilar has to run clinical trials to prove the outcome matches that of the biological it’s imi- tating even despite being structurally different.
3
Why shoul* a Fami*y Medicine doctor know about bio- similars? Biologicals are very expensive and proprietary molecules. Their make-up and manufacturi*g details are usually closely guarded secrets. Biosimilars on the other hand are imitations that can be produced with much less
PROCALCITONIN
Procalcitonin [PCT] is a precursor of the hormone calci- tonin which plays a role in calcium metabolism. PCT does not affect calcium metabolism and in healthy per- sons it is virtually undetectable. First identified in 1970, it is on*y in the later years its significance came to be known in states of bacterial infections of the lung and sepsis. PCT is produced by the parafollicu*ar cells of the thyroid gland and by the neuroe*docrine cells of lungs and intestines. The levels of PCT steeply go up in inflam- matory stimulus of bacterial origin and not of viral or other inflammatory states. In bacterial lung infections it is the neuroendocrine cells that produce PCT.
FIBROELASTOGRAPHY
Establishing the presence of fibrosis or cirrhosis in pa- tients with chronic liver dis*ase is important for assess- ment of prognosis and for evidence of progressive disease (fibrosis) in disorders such as hepatitis C virus (HCV) in- fection, hepatitis B infection, or non*lcoholic fatty liver disease. Till recently, liver histology obtained by percuta- neous liver biopsy is the "gold standard" for the presence of fibrosis or cirrhosis. Liver biopsy carries a small risk for the patient, may be associated with procedure discomfort, and interpretation can be affected by sampling error and interpreter variability.
Elastography, known as FibroScan, uses a modified ultra- sound probe to mea*ure the velocity of a shear wave cre- ated by a vibratory source. Estimates of stiffness of the liver by ultrasound correlate with fibrosis stage. Ultrasound elastography can be performed in ap- proximately 95% of patients, although older patients and pati*nts who are obese can be more difficult to study. This technique has been evaluated most consistently in pa- tients with chronic HCV disease.
Ultrasound elastography is strongly correlated with ad- vanced fibrosis in patients with chronic hepatitis, and val-

expense but with sim-
ilar efficacy. Hence
they have a potential to *ignificantly lower cost and in- crease access for our patients with serious illnesses.
When one is faced with the problem of differentiating say pneumonia caused b* a virus or bacterium, test for PCT levels will help the clinician to avoid or stop antibiotics if the levels are normal. Another interesting feature is that the rise in PCT levels will not automatically cause a rise in calcitonin levels, giving rise to the question whether this prohormone has an independent role to play. The test is more sensitive than tests for other markers of in- flammation like IL2, IL8 and TNF alpha. This test is available in our city.
ues above 12.5 kPa are indicative of cirrhosis. This tech- nique works best for separating patients with minimal or no fibrosis from those with significant fibrosis. A linear correlation with i*creasing fibrosis has not been demon- strated, and 15% discordance between elastography scores and histologic fibrosis has bee* observed. Advanced fibro- sis may be underestimated and patients with macronodu- lar cirrhosis may b* classified as noncirrhotic. Fibrosis may be overestimated in patients with extrahepatic ch*- lestasis or acute hepatocellular injury due to the effects of these conditions on liver stiffness. Ultrasound elas- tography does not distinguish patients with no fibrosis from patients with minimal fibrosis. Ascites can interfere with the generation of a shear wave through the liver.
In summary, ultrasound elastography will separate pa- tients with minimal or no fibrosis from those with ad- vanced fibrosis or cirrhosis, although it may occasionally underestimate fibrosis in some patients with advanc*d fibrosis or macronodular cirrhosis. Additional studies will establish t*e role of this technique in evaluating hepatic fibrosis in patients with chronic liver disease. (Source: Medscape)
4
TUBERCULOSIS: CLASSIFICATI*N BASED ON DRUG RESISTANCE

Drug sensitive TB. Here the TB bacillus is sensitive to the first line of antitubercular drugs.
Drug resistant TB is further classified into:
-
Mono resistance
-
Rifampicin resistance
-
Polydrug resistance
-
Multidrug resistance
-
Extensive drug resistance
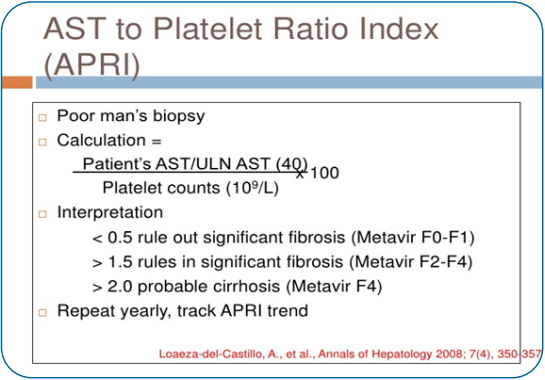
APRI SCORE
This is another important tool to assess liver fibrosis. The calculation is based on platelet count and AST levels and has a high predictability as to the extent of liver damage.
Our online learning program every alternate Friday night has been very successful so far. To participate as a faculty / Con- sult*nt please contact Dr. B C Rao or Dr. Jaya Bajaj.
CASE REPORTS
A CASE OF PARATHYROID ADENOMA
It is customary to ask for serum electrolytes among other tests, in patients who come with complaints of nausea and vomiting, bod* aches and other vague constitutional symptoms but not serum calcium. Elevated serum calci- um is always abno*mal and can occur in number of con*i- tions, some of them not all that uncommon in every day practice. All types of malignancies, lymphomas, multiple myeloma, cancers of colon, rectum, prostate and lun* can raise the serum calcium levels. So in catabolic states of thyrotoxicosis, AV shunts, osteoporosis, excessive intake of Vitamin D and increased absorption as in milk alkali syndrome and sarcoidosis. In these states the increased
levels of serum calcium leads to a negative feedback and resu*ts in low levels of parathyroid hormone. The reverse happens in primary parathyroid disease when there is increased or normal levels of PTH [parathyroid hormone] with hyperplasia or a frank secreting adenoma of the par- athyroid gland. This is called primary parathyroidism.
Following is the report of such a case which presented with suggesting clinical features but still went undiag- nosed for months because this simple test of serum calci- um was not done.
5
Mr S, a 6* year old gentleman whom I know, went to his doctor at Mangalore on 15/2/13 with compl*ints of inter- mittent fever of 5 days, nausea with vomiting of 3 weeks and weight l*ss of 5kgs of two months duration. After examining the patient the doctor asked him t* get some tests done. Patient went back to the doctor on 18/2/13 with the reports. His blood studies were normal so was his blood glucose level. Widal test was negative and urine analysis was normal. Liver function te*ts revealed border- line increase in SGPT, SGOT and alkaline phosphatase. His ESR was 40mm. As he did not get better [details of treatment not available] he went to another institution based doctor and some more tests were done. The case notes showed his BP was 160/100 and temp was 99.8F, ESR 60mm, PSA levels were normal, Blood for Filaria was negative. Monteux test was strongly positive. He was started on antiemetics, IV fluids, and antibiotic oframax (Ceftriaxone) 1*m twice a day. The treatment continued till the first week of March with marginal benefit.
On 10*3/13 an abdominal ultraso*nd was done which showed a 21 mm size cyst in the left lobe of liver, m*ltiple calculi of 15 to 17 mm diameter in the gall bladder, grade II bilateral renal parenchymal changes and minimal thickening in the anorectal region. On 13/3/13 a lower GI endoscopy was done which was normal except for a rectal prolapse. Urea was 65 mg/dL and creatinine was 2mg/ dL, electrolytes were normal.
This was the time, given the findings of weight loss, con- tinuing fever, strongly positive Monteux, high ESR and renal findings, the possibility of Koch’s infection was con- sidered and empirical treatment was about to be started. Patient took the decision to come to Bangalore and seek help. When I saw him on 22/3/13, what struck me was the severe cachexia w*th loose folds of skin hanging at his neck, arms and abdomen. His BP was 160/100 with * heart rate 0f 100, temperature was normal, tongue was

bald, no nodes were
felt in the neck, axilla
or groin, heart and
lungs were normal. Abdomen felt doughy and there was rectal prolapse which coul* be pushed in. In m* mind I thought I was dealing with some kind of malignancy. I too asked for some tests and the results on23/3/13 were: Hb% 12.9,ESR 97mm, WBC 11,700 with Poly 81,Lymph 15 and E 4, creatinine 3.64, T4 6.25, TSH1.32, B12 432pcg.
He was ask*d to keep a temp record, was given dulcolax suppositories and asked to report back in three days. On 25/3/13 he said he felt better as there was no fever but he continued to have nausea, loss of appetite and vomited occasionally. With this history of weight loss and upper GI symptoms possibility of gastric cancer was thought off and he was asked to undergo upper GI endoscopy which was duly done and found normal. At this stage, LFT, se- rum protein electrophoresis and CT abdomen were ad- vised and done.
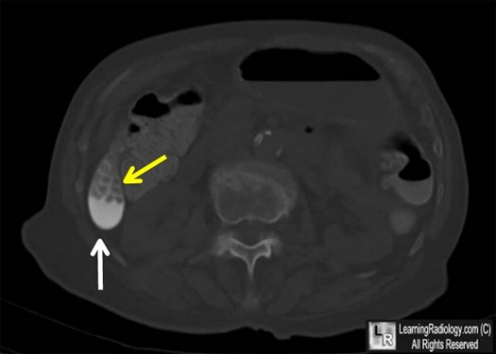
CT findings: Milk of calcium bile in the gall bladder with multiple small cysts in the liver LFT revealed alkaline phosphatase levels to be 205 [high], GGT levels 60 [border line high]
Finding milk of calcium in the gall bladder made me ask for a serum calcium still keeping malignancy [occult] in mi*d. On 29//13 the lab reported serum calcium levels to be 16.6 [8-10.5 N]
Patient was ha*ing nausea, vomiting, constipation, renal involvement, raised serum calcium levels, increase in phosphatase levels. Could he be having secreting parathy- roid adenoma? A serum paratharmone [PTH] estimation was done on 2/4/13. It was 1616 pcg and serum calcium was 19.5mg dl. Both way above normal.
Clinical diagnosis of secreting parathyroid adenoma was made and the pati*nt was referred to the oncosurgeon who specializes in minimally invasive radio guided para- thyroidectomy.
He was admitted and this procedure was done on 10/4/13.He was discharged on 13/4/13.
Since then he has come for three follow ups. His acute symptoms of nausea, vomiting, constipation rapidly abat- ed. His weight gain too was rapid. Rectal prolapse sponta- neously became normal. Renal parameters took one year to return to normal and so was his blood pressure.
6
Some unusual features. Though one finds reference to fever this is not a presenting feature of parathyroid ade- noma [primary hyperparathyroidism]. In this patient presence of low grade fever led to all kinds of tests and even made the attending doctors think *f Koch’s infection. The other unusual feature is the finding of milk of calcium in the gall blad*er (see CT image above). This is also a rare finding. More often than not patients with hy- perparathyroidism present with renal calculi.
And it is said that nearly 15% of patients presenting with calcium stones in the kidney will have hyperactive para- thyroid gland. The classical description of moans [tiredness], groans [abdominal colic] and stones [urinary calculi] is an apt description for primary parathyroidism.

Standard text books
don’t feature milk of
bile in gall bladder and
fever in the signs and symptoms of primary hyperparathy- roidism.
Those of you who are interested in knowing the fascinat- ing operative details of minimally invasive radio guided surgery for this condition should visit the website of Na- tion*l Medical Journal of India 2007/Jan/Feb and look for article by Dr. S. P. Somasekar et al.
Dr. B. C. Ra*
PRACTICE EXPERIENCES
DIABETIC MITRA INSULIN BANK — MAKING INSULIN THERAPY PATIENT FRIENDLY
Dear friends, I am introducing one of my initiatives, Dia- betic Mitra Insulin Bank to you. It is self-funded to mak* life of diabetic patients easy and healthy by treating them well in time with early identification of complications and preventing them.
D*ring the journey of this p*oject I realized many of my patients were afr*id of using insulin as a therapy option. Reasons were, fear of insulin injection, dependency, long duration of therapy, cost and non-availability of *asy de- vices like insulin pen. Keeping these difficulties in mind we thought of starting a bank where patients will get eve- rything that is required for insulin therapy, both conven- tional and modern. This bank *ives patients options to pre -deposit money and book the requirement in advance or buy later as per need. This move helps patients during times of crisis like lack of salary, drought or flood situa-
tions. We kept this channel open because when patient runs out of money he/she avoids taking proper medica- tion and later lands up with severe complications. We hope this initiative will reduce the damage to some extent.
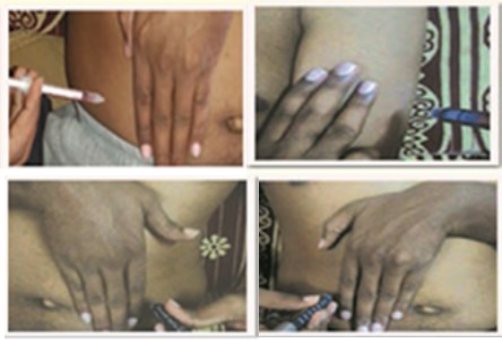
This initiative is running on a very positive note and Mr. Manjunath is our strong support like reserve bank. Till date we have 20 plus members utilizing our services. Un- der this initiative we also pay lot of attention to insu*in administration and counselling. During consultation we spend lot of time with patients, try to reduce th*ir fear about therapy as much as possible, teach them appropri- ate ways of administration with the finger rule.* We also encourage them for self-insulin administration. With help of finger rule the chances of insulin going intramuscular is reduced and it becomes almost pain free.

*3 finger, 4 finger, 5 finger rule
7

In the future, we hope to start a patient support fund which will help needy type 1 Diabetics, elderly and poor patients who are on insulin therapy but cannot afford to get it due to financial or family problems. We also hope our work will reach maximum population and we will succeed in spreading message – ‘Let’s Live Healthy with Diabetes’.
While taking insulin over the arm patient should keep 3 fingers over biceps and triceps, then remaining area is
HOT TEA AND CHES* *AIN
Mr. Ramesh is a good friend and also a patient, a dreadful combination. He came to me complaining of chest dis- comfort and insisted that it was due to drinking scalding tea that morning. Ignoring his diagnosis, I started asking him the usual questions we doctors ask to exclude pain due to heart disease. Where was the pain, did it go up to *he neck and down the arm, was there any sweating, how long did it last, etc.
When I was asking these questions, he sat there giving me a bored look. I knew what was going on his mind. ‘I came here with some trivial problem and this fool is asking me these stupid questions. He looked at his watch twice in those few minutes I spent trying to get a proper history.
Despite his protests, I did a cardiogram. The tracing showed severely compromised blood supply to a portion of the heart. I explained the gravity of the problem, gave him a note for hospital admission, called the cardiologist friend of mine and sent him on his way.
The same afternoon I went to the hospital to see him. I went directly to the coronary care unit. I did not find him ther*. Then I went to my cardiologist friend to find out what had happened. Before I could open my mouth, he asked me, ‘where is your friend?’ Having made sure that he was not in the hospital a*d worried, I called his office

ideal for insulin ad-
ministration. They
can take it laterally-
when arm is put in supine position. This helped us to overcome the fear of inj*cting into the deltoid muscle. Over abdomen, we *sked patient to leave 4 finger area from umbilicus. This *eads to sparing of rectus sheath and facilitates administration of insulin subcutaneously. So here patient can rotate sites easily. Over thigh we used 5 finger rule, so patient spared quadriceps and hamstrings. Patient can take insulin over tensor fascia lata or adduc- tor compartment if he follows this method. But here chances of absorption via intramuscular route are higher. Hence the thigh is not an ideal site.
Dr. Smruti Haval Nikumbh, Family Physician, Sankeswar. Email: drsmrutinikumbh@gmail.com
only to b* told by his well-meaning secretary that he was fine but in a meeting and would I mind callin* him after an hour or so? The knowledge that he was alive was reas- suring but all the same the worry was no less.
I went to his house to apprise his wife about the serious nature of the problem. I found her having her prized af- ternoon siesta. After I finished my tale regarding her hus- band’s erratic behavior, she gave me a splendid piece of advice. ‘Doc, you always worry too much. He gets these pains after drinking hot tea. You have advised him to stop this bad habit [I did not remember this piece of expert advice having been given] and if he does that, he will be OK, you wait and *ee!’ I requested her to please send her husband to the hospital without wasting any more time, drank t*e cup of tea which she made and returned home thoroughly depressed and worried.
Are you wondering wha* happened to my friend? He did- n’t want to go to the hospital, especially no* when all the pain had gone and he felt very good. He made an unevent- ful recovery. *is subsequent ECGs showed a small scar and his treadmill test came back negative. According to his wife, he gets no chest pains now because he has stopped drinking hot tea. No credit whatsoever to the poor me who spent several sleepless nights and anxious
8
days looking after an unwilling and, I suspect not very grateful patient! Even now he says he takes the medicines to keep me in good humor!
A YOUNG DOCTOR’S NIGHT
Though young doctors during their tr*ining years learn how to diagnose and manage illnesses, it is only after col- lege years and during their internship they face the hu- man face of diseases. Following story is one such.
It was very early in my career, I had joined Jayadeva In- stitute of Cardiology, to get some hands on training in cardiology and was on my first night shift. I with the help of three nurses and one ward boy had to take care of 20 patients on beds and some more on stretchers and trol- leys. This night shift could well be called grave yard shift as lots of patients with acute heart disease would succumb despite our best efforts.
This was also the time, when I was engaged to be married and life appeared beautiful and happy. It must have been around 1 am that we received a call that a patient with his ECG showing acute anterior wall MI with dropping BP. The patient, a 35 year old man was wheeled in to the ward on a stretcher accompanied by his young wife. We quickly hooked him on to the monitor and I worked on the usual emergency protocols.
The patient asked the nurse if he could go to the loo. The nurse looked at me and we shared our secret coded look. Here we believed that if any patient asks to go to relieve his bowel in such emergency situation (w*th no recordable BP) will not survive the next 15 mins. The nurse offered to help him with a bed pan. The wife and the patient were having a silent conversation with their eyes. The wife spoke up and said ‘you are leaving me alone and going’, to which the husband though breathless said he wanted to see his son. With the doctor and nurse working on him, he seemed to know he did not have much time left. We asked the lady to wait outside the ICU. A while later the patient passed away.
I had to break the sad news to his wife and I was emotion- ally drained and felt unfit to do so. Luckily I saw a trainee cardiologist who was passing by after reviewing a differ- ent *atient. I requested him to break the news to the pa- tient’s wife, thinking he will make it less painful for her. I followed him outside the ICU where the lady was sitting on the floor ignoring the chairs. He called to the lady and told her, ‘Amma, your husband is dead, you can take him
Dr. B. C. Rao, Family P*ysician, Bangalore E m a i l : b a - dakere.rao@gmail.com

back’ and he walked away leav*ng me aghast. I rushed to the lady try*ng to do damage control, but was surprised that she was neither sad nor crying. I could only see worry on her face. I asked her if she was alright and if she need- ed any assistance. Since the hospital bills were not a wor- ry, I wondered what was bothering her. (In such emergen- cy cases, the hospital would waive of* all expenses).
She then narrated that she and her husband reside at Ko- lar and were visiting Bangalore to attend a wedding. The night before, they were waiting in a bus stop to return home, when her husband felt the discomfort in the chest and collapsed. Passersby had helped them in shifting to the hospital in an auto rickshaw. Now that she is in the hospital and her husband no more, she was worried as to how she would return home to Kolar with a dead body. She had no money or contacts here. She didn’t even have any phone numbers of her kin whom she could call and ask for help. Those days, in 2005, mobile phones were not common and affordable.
The nurse asked the ward boy to check the wallet of the p*tient and see i* there were any details of contacting someone back home. He did find a number among lot of debris in the pocket. The kind ward boy used his personal phone (back then we were very conservative about spend- ing on cell phone) and made the call. It turned out to be some iron and steel dealer who didn’t know the patient. He only vaguely remember*d someone by the patient’s name and passed on a different number to contact and see if it helped. T*e ward boy was lucky this time as it turned out be the deceased’s brother’s number. The rest after that was e*sy as the brother came down and helped the lady.
I being fresh in my medical career, entering into new life, was shown life’s uncertainty at such an unearthly hour. The piercing stare and the mute exchange between the couple, the lady’s response to the bereavement have left a lasting impression and that young woman’s worried face, even now so many years later, continues to haunt me.
Dr. Syed Abu Sayeed Mubarak, Family Physician, Banga- lore. Email: drsyedabu@gmail.com
9
A TALE OF CALM PATIENT AND TENSE DOCTOR

Mr. N’s daughter called me around 8 AM. I was brushing
my teeth and answered the call. She said, ‘father says he is not keeping well a*d wants to see you. What time shall
I ask him to come?’ I said ‘around 9:30 AM’. She hung up. Neither did she tell me what the problem was nor did
I ask as I was in the middle of brushing my teeth! thought it will be for his usual cold, cough, and fever.
I know Mr. N and his family very well for the last 4 years, since I started my practice. I have been consulted on many occasions for health problems of his *ife, daughter, son in law, and his two grandchildren. He is 71 year old and comes to see me frequently for minor problems such as, cold, cough, and fever or for his blood sugar and for BP checkup. He is a diabetic since 10 years on OHA and is well under control and his seasonal cough lasting few weeks. He usually does well with SOS use of duolin inhal- er.
I was doing a dressing for a diabetic wound when he came to my clinic around 10:30 on his moped. After I finished, I opened the door and saw him sitting quietly .
It is unusual for him to come and sit silently without maki*g an announcement of his arrival in the clinic either *y peeping through the door or walking restlessly in front of semitransparent glass door of the co*sultation room. Sometimes he would walk in even if there are pa- *ients waiting and I have to pacify the waiting patients! But this time I was surprised to see him so quiet.
He walked in slowly and sat on the chair. I asked him ‘what is the problem?’. He said he was feeling slightly tired since 2 days and had wheezing early in the morning around 2 AM w*i*h troubled him for 2 hours and after using duolin inhaler he felt better. He could go back to sleep around 4 AM. He woke up around 8 AM and asked his daughter to find o*t my availability. I enquired whether he has cold, fever, chest p*in, dryness of mouth, increased urination, vomiting, loose stools and he denied any of those symptoms. I then examined him. His tongue was moist, temperature was normal. His pulse was fast, more than 150 per minute but regular, and his BP was 90/70 mm Hg. I got worried and thought that I will make him lie down on the examinatio* table for 5 minutes and recheck. For a change, he appeared calm and quiet but I was tense and restless! After 5 minutes of rest there was
10
I
no change. Pulse oximetry was showing pulse rate of 187 per minute. His blood sugar was 246 mg/dl. I do no* have an ECG machine in my clinic. He had come alone. There were three patients waiting outside. I requested them to *ait for half an hour and took Mr. N in my car to a nearby hospital which is 10 minutes’ drive. On the way, I told Mr. N that there is some problem with his pulse and we will do an ECG and check. He was quiet and did not appear disturbed and said ‘ok, do as *ou feel right’.
I briefed his details to emergency medical officer and im- mediately took an ECG which showed supraventricular tachycardia. Despite a few minutes of carotid massage, there were no changes in the ECG. Adenosine 6mg IV was administered with which the rate returned to normal.
After few minutes I went outside to inform his daughter, who was out shopping in the city and she said she will come in fifteen minu*es. I waited in emergency at his bedside watching over Mr. N. The daughter came alone and I introduced her to eme*gency medical officer and explained her father’s problem and showed her the ECGs. She understood but the seriousness of what her father had gone through did not sink in, as her father was look- ing fine! She said “you know it better”, and asked what next? I said he will be here for a few hours and we will take a cardiologist’s opinion and if he says ok then you can take him home. She phoned her husband who was waiting outside on a two wheeler and he said let us go home and send your mother to the hospital. He did not like his in-laws and he had told me that. She cried silently and told him to go home and she will stay in the hospital. I went back to my clinic at 12 PM to see the waiting pa- tients. Meanwhile I forgot to pick my son up from school at 12:30 PM.
The cardiologist suggested electrophysiological studies and angiogram and sent him home on metoprolol. I went to see him later at 10 PM on his moped which was still parked outside, after finishing my cli*ic and checked him once to make sure he was doing well. His daughter and son in law were out for another round of shopping! My wife picked me up from his house.
Dr. Ravikumar Kulkarni, Family Physician, Mysore Email: ravikumarkulkarni@yahoo.com
RESIDENT’S CORNER
MY EXPERIENCE IN FIRST YEAR RESIDENCY

While I was planning to write this essay, I realized I have just completed my first year residency in Family Medi- cine. It has been a year filled with joy, struggle, str*ss, achievement etc. At the outset I must confess that I am not a newcomer. I came in with a year of experience *n critical care medicine, half a year training in family medi- cine, and more than a year training in triba* health care. So I had chosen what exactly I wanted in the DNB en- trance exam, and God obliged my request.
It was during pre-PG t*mes that I came across this won- derful organization called AFPI. Why I call it wonderful? Simple - it was in February 2016 that two conferences were conducted back to back in the name of Family Medi- cine, in my quest to collect credit points I attended both of them. After attending the one conducted by AFPI, I walked out with a mind filled with reasoning and ponder- ing about previous experiences, and I call it Continued Medical Education (CME). While in the other one I walked out with hands filled with goodies not so useful to me, and I call this one Continued Medical Socialization!
Thesis is considered to be a dreaded assignment for the resident. Though I started on day 1, it t*ok me more than 6 months to submit my protocol. The reason being I kept changing my topic from psychiatry in general practice, to commu*ity based malnutrition rehabilitation, to end of life care in critical care, to finally stress among adoles- cents.
Some of my postings during my residency were quite in- teresting. It was during my o*tho*edic postings, I realized the worth of family medicine in specialty postings. I was the first person to pick up urosepsis in a post-op patient
and central respiratory depression in a patient with diaze- pam overdose (given as a muscle relaxant) during ward rounds.
Community postings were pretty interesting as you have hands on experience. Once it so happened that I posted a patient for lipoma excision in critical area of face between facial nerve and the eye. To my bad luck, after skin inci- sion I realized that the instruments with me are either blunt or bigger in size. It was when I finished the proce- dure with great struggle that I realized that many more such situations are bound to appear during our practice.
Attending the National conference by AFPI was a dream come true, as I had to go through a series of barricades bef*re me. It was in the conference I learnt the different facets, philosophy, need, and opportunities of family med- icine. It helped me in preparing myself for times when I face critique or query abou* family medicine.
We first year residents in family medicine formed a team to participate in the TB quiz. Being underdogs, we gave stiff competition to the experienced specialty teams. Though we came runners up, it was certainly a confidence booster.
Overall, while my life is going through a rough phase both personally as well as physically, *t was the association with Baptist hospital and team AFPI that I am still breathing life.
Dr. Vivek Karthikeyan, Family Medicine Resident, Baptist Hospital. Email: viveksoukya@gmail.com
Welcome to AFPI Karnataka http://www.afpikarnataka.in
11

MASALA
The village was in deep trouble. The cat population was beyond control. They could be found everywhere and one *ould not take a step without tripping over one. They were found on the roads, window sills, compound walls, tree branches, roof tops and visited the insides of the houses as though they owned them.
Villagers tried trapping, getting hunting dogs, scaring tactics like explosives with very little success and the cats continued to ru*e the roost in the village. It was this *tage when they got hold of the news of a cat eliminator who was very famous and had the advantage of speak- ing the cat language. A delegation of villagers went to meet up with him and settled on a fee to get him over to come to their village and catch the cats. On the designat- ed day the VIP eliminator arrived with much fanfare and he was taken on a tour of the village. After the tour the eliminator pointed to one well-built, superior look- ing tom cat perched on the branch of a nearby tree and said, “that *ne, he is responsible for this, he is a prolific breeder and I will catch him and sterilize him, your problem will be over”.
He proceeded to entice the tom cat into a trap, duly ste*- ilized him, collected his hefty fee and went his way. The matters were quiet for a while and it appe*red that the numbers were on the decline. But once again the num- bers began growing and the problem became worse. The delegation went to the cat eliminator and com- plained. He too was surprised, he said, “this is the first time this has happened, I will come and see what has gone wrong”.
He went to the village and once again toured th* village. What the villagers said was true. The cat population had indeed increased. He found the villain cat sitting on th* same tree branch grooming himself with that supe- rior look. He went and asked the tom cat, “How come your numbers have increased despite my surgery on you?”
The tom cat replied, ‘I have now become a consultant’! (No pun intended !)
12