May 2018, Volume 2 / Issue 1
AFPI Karnataka Quarterly Newsle*ter
President’s Letter
It’s been a good eight years since we came together as a team and formed the Academy of Family Physicians of India (AFPI*. Karnataka State chapter was formulated three years ago with an objective of carrying the vision of AFPI to promote Family Medicine, to meet the educational needs of family practitioners and to work towards reforming the
Health Care system. There had been a growing frustration among family physicians,
confusion among the public about the role of family practitioners, and continuing ineq- uities and inefficiencies in the Indian health care system. Need was felt to revive the dy- ing art of Family practice to meet the basic health care needs of the community in a changing health care environment.
Although the ground situation has not changed significantly, there definitely are some comforting facts for the young FPs to feel reassured and optimistic. Public percep- tion has definitely moved towards the trustworthy ‘Family Doctor’ who they feel could resp*nd effectively to their basic health care needs. Enhanced investment in the primar*
care sector has opened up a lot of job opportunities with decent pay packages. Hospital
administrators have realized the value a qualified family physician could bring in across the spectrum of health care facilities. Insurance companies ha*e started including OPD services in their scheme of things. Medical PG aspirants have started considering Family *edicine as a specialty of choice. More than anything we can see a sense of pride among Family Physicians in what they are doing as professionals.
Having embarked on these positive developments, one is aware that it is an enormous task to retool the specialty and reform the health care system. Regrettably, we have not been able to make significant inroads into policy implementation in the gov- ernment health care sector. The outcomes of any constructive effort is highly dependent on the ensuing input, critique and conviction demonstrated by the family Physicians fraternity themselves.
I must admit that I am very excited and fortunate to be part of AFPI Karnataka for the past three years. Excited* as there is still much to do because there is a lot hap- pening in the health care ecosystem that we can contribute to. Fortunate, because we have a very vibrant & capable team which allows me to look at the tasks ahead with con- fidence.
The Nephro-Urology CME held last month was a grand success with interesting session* generating meaningful interactions. OSCE workshop was conducted for DNB Residents at Bangalore Baptist Hospital. We have some important events lined up for the next quarter. Hope to see some of you at the WONCA World Rural Health Confer- ence at New Delhi from 26 *h to 29 th April. We are in the process of revamping our web- site to make it interactive and resourceful. Looking forward to your active contribution in all our endeavors and valuable feedback as always.
Col (Dr.) Mohan Kubendra
President
Col (Dr.) Mohan Kubendra mohankubendra@gmail.com
Secretary
Dr. Bhaskara Puttarajanna drbhaskarap@gmail.com
Vice President dr.rk.prasad@gmail.com
Dr. Ramakrishna Prasad
Treasurer
Dr. Ravikumar Kulkar*i ravikumarkulkarni@yahoo.com
Scientific Chair Dr. Jaya Bajaj
jayabajaj@gmail.com
Editorial team
Dr. B. C. Rao badakere.rao@gmail.com
Dr. Roshni Jhan Ganguly roshnijhan@hotmail.com
Dr. Ramakrishna Prasad dr.rk.prasad@gmail.com
Inside this issue
|
AFPI News |
2 |
|
Gleanings |
4 |
|
Case Reports |
9 |
|
Practice Experien*es |
14 |
|
Announcements |
16 |
Editorial Note

There is an argument in some quarters that a family medicine specialists work should be entirely in the community. In contrast, the role of the specialist is expected to be in an institution or a hospital. This kind of thinking is detrimental to the development of both the disciplines.
A competent family medicine specialist can look after many patients under his care if they need ad- mission, in a hospital. To give a few examples, high fevers, pneumonias, gastroenteritis, normal de- liveries, problems needing day procedures and such. If this is done it is a win-win situation. It is al- so mutually *eneficial to FPs and to hospital-based doctors as they will appreciate each other’s ap- proach to a given problem and will reduce the patient burden on the subject specialist. The problem FPs face and are facing is restrictive policies adopted by institutions and time management.
What about hospital-based doctors? Visiting patients in their homes and doin* OPDs in the com-
munity set up will help them understand the unique problems the FP faces and solves in *h* com-
munity setting. They will also appreciate that man* problems presently managed in hospitals can be managed as efficiently or even better in the home setting. It will also bring them down from their ivory towers and expose them to the socio-economic realities of life outside the hospital set up.
This arrangement will help make both hospital based and community-based doctors understand and sympathize with each other when faced with patient related issues.
AFPI News
AFPI Karnataka OSCE Workshop at Baptist Hospital
OSCE workshop was conducted for DNB Residents at Ban- galore Baptist Hospital* This program *as led by Dr. Srividhya Raghavendran and Roshni Jhan-Ganguly along
wit* other faculty at Baptist hospital. A large number of res-
idents from Bangalore and out*ide participated in this well organized event.


2
A*PI News
T*e AFPI Karnataka Nephro-Urology CME was held on the 25 th of Feb, 2018 at NU Hospital. A range of topics of relevance to family medicine practice including manage- ment of u*inary tract infections, chronic kidney disease,
dialysis, hematuria assessment, and incontinence were
addressed. High quality interaction ensued following the presentations.




3
Gleanings
No CVD Benefit With Omega-3 Fatty Acids Source: Medscape Cardiology
A recent m*ta-analysis by Clark et al that included several
high-profile trials, such as ORIGIN, JELIS, GISSI-HF, and GISSI-P—all with at least 500 participants and an average duration of 1 to 6.2 years. All but one trial tested a daily dose of omega-3 FA of 226 to 1800 mg of eicosapen- taenoic acid (EPA) and 0 to 1700 mg of docosahexanoic acid (DHA), with one using 1800 mg/d EPA alone has concluded that: "There are no beneficial effects of treatment with omega-3 FA on any CVD, or on any subtype of CVD, or on any CVD in any sub-
group of the population."
This meta-analysis is different from previous meta- analyses in that it assessed the effects of omega-3 FAs on prespecified CVD subtypes and CVD in a range of patient populations. Nevertheless, the authors write that the 95% CIs in the analysis "cannot exclude a 7% lower risk of ma- jor vascular events and a 10% lower risk of CHD associat- ed with omega-3 FA supplements." About 23% of partici- pants had prior CHD, prior diabetes, total cholesterol of 193.1 mg/dL or greater, or triglycerides greater than 150.4 mg/dL, and about 15% reported prior statin use.
Clarke observed that two large ongoing trials—VITAL in the United States and ASCEND in the United Kingdom— will provide additional evidence later this year on the ef- fects of 1 g o* omega 3 FA per day in a further 40,000 pa- tients.
In the light of the consistent null findings from the 10 pre-
vious trials, there is little expectation that the results of the ongoing trials will differ from the results of the pre- sent m*ta-analysis. VITAL principal investigator, Dr Jo- Ann Manson (Brigham and Women's Hospital, Harvard Medical School, Boston) said in an email, "When effects of an intervention remain inconsistent and inconclusive de- spite extensive study, it is often because effects are mod- est in the populations tested."
In the case of omega-3 FAs, the agents have been tested
predominantly in secondary prevention and high-risk populations, often in the setting of concomitant use of other medications, such as *spirin, statins, ACE inhibi- tors, and β-blockers. Also, many of the trials were of short duration and tested low doses, she said.
A key unanswe*ed question is whether marine omega-3 FAs reduce the risk for MI, stroke, CV mortality, and oth- er CVD events in a primary prevention setting, among
those at "usual" risk of CVD.
VITAL, the first such large-scale randomized trial, is be- ing conducted in 25,874 participants who were selected only on age (men aged 50 years or older and women aged 55 years or older), were free of CVD at baseline, and did not have high use of aspirin or statins (l*ss than 50% for each). The mean trial duration is 5 years; results are ex- pected this fall. Other trials, such as ASCEND, DO-

Some concern has been expressed that patients in VITAL may be too healthy, controls may have decent omega-3 levels, and event rates may be low and called for further research with 2 to 4 g/d omega-3 FA in CHD and HF. While awaiting additional data, patients are still advised to eat fish at least two per week but taking fish oil supple- ments has no beneficial effects.
Oral Eczema Treatments Generate Excitement
For patients with atopic dermatitis, oral medications could replace injections if dramatic results from two phase 2 trials are confirmed. "It's a very exciting time," said Emma Guttman, MD, PhD, from the Icahn Sch*ol of Medicine at Moun* Sinai in New York City, who presented
results from a phase 2 trial of upadacitinib (AbbVie) here
at the American Academy of Dermatology 2018 Annual Meeting, where a similar trial of baricitinib (Eli Lilly) was also presented.
"For many years, patients didn't have safe treatment," she told Medscape Medical News. "The only approved *ral treatment in the United States is prednisone, which has terrible side effects for long-term use. And many times, when you stop it, the disease comes back even worse."
The new oral drugs have yet to be compared directly with each other, o* with injections of dupilumab, *ecause no head-to-head studies have been conducted and the study designs *re different, said Guttman, but results have been encouraging enough to raise hopes about a comparable effect.
Dupilumab "revolutionized" the treatment of moderate to severe *topic dermatitis, she explained. In the identical
SOLO 1 and SOLO 2 trials (N Engl J Med. 2016;375:2335-
2348), about half the patients achieved a 75% improve- ment in Eczema Area and Severity Index score (EASI-75) af*er receiving injections every other week for 16 weeks. In the SOLO studies, the incidence of herpes vi*al infec- tions increased and 7% to 12% of patients receiving dupi- lumab developed conjunctivitis, but neither of these ad- verse events was considered serious, said David Eric Co- hen, MD, from New York University in New York City, during his overview of new atopic dermatitis treatments at the meeting.
Both upad*citin*b and baricitinib work by inhibiting Ja- nus kinases (JAK), rather than interleukins, and neither is considered to be a biologic becaus* the manufacturing is conventional; the drugs are not created in cells, as biolog- ics such as dupilumab are.
4
Gleanings
Upadacitinib Study
In the upadacitinib st*dy, the 166 participants were ran- domized to once-daily monotherapy with upadacitinib 30 mg, 15 mg, or 7.5 mg, or placebo. At 16 weeks, signif- icantly more patients in the upadacitinib groups than in the placebo group achieved EASI-90 and an Investiga- tor Global Assessment (IGA) score of 0 or 1, indicating complete or almost complete resolution of symptoms. And in the upadacitinib groups, improvements in itch were huge.
Baricitinib Study
The approach was slightly different in the randomized trial of oral baricitinib. The 124 participants were al- lowed to apply topical cortico*teroids while they re- ceived once-daily baricitinib 4 mg, 2 mg, or placebo. Symptom im*rovement was better in the baricitinib groups than in the placebo group. And more patients in the 4 mg group than in the placebo group achieved an
EASI-50 at 16 weeks (61% vs 37%). Improvement in 28-
point Patient-Oriented Eczema Measure (POEM) scores were better in the 4 mg baricitinib group than in the placebo group (–7.5 vs – 3.5; P = .011), and in the 2 mg group than in the plac*bo group (–6.4 vs – 3.5; P = .07). Treatment-emergent adverse events were reported by 71% of patients in the 4 mg group, 46% in the 2 mg group, and 49% in the placebo group. "In a nutshell, baricitinib worked quite well, particularly for itch and sleep disturbance," said Jonathan Silverberg, MD, PhD,
MPH, from Northwestern University in Chicago, who
presented th* findings. "And in a subset of more severe patients, we saw even better results."
This study also established a dose–response effect, he told Medscape Medical News. "There was a clear bene- fit for 4 mg."
Note: The upadacitinib t*ial was funded by AbbVie. The baricitinib trial was funded by Eli Lilly.
Source: American Academy of Dermatol*gy (AAD) 2018
Annual Meeting: Abstracts 6684, *533, *nd 6658. Pre- sented February 17, 2018*
Interpretation of Thyroid Function tests. Com- mon pitfalls. Management of Hypothyroid state
Although in most cases interpretation of thyroid func- tion tests is straightforward, unusual conditions can generate unusual patterns [of thyroid function tests]
which can be difficult to interpret. As general physi-
cians, we should be aware of these pitfalls and adopt a practical approach in dealing with Thyroid dysfunc- tions. In many cases, correct diagnosis of rare thyroid conditions based on their thyroid function tests has very important implications [for the management of individ- ual patients and their family members]. With the excep-

tion of detailed genetic analysis, the tests required to investigate and diagnose are easily available. The chal- lenge lies in applying them to the right individual and at the right time.
Choosing the right thyroid function test
The choice of first-line thyroid function tests depends on local arrangements and laboratory protocols. TSH is a highly sensitive test and using it as a single criterion has been shown to accurately classify the thyroid state of a patient in over 95% of cases. An abnormal TSH is the first abnormalityto appear in thyroid disease, where other thyroid tests can be normal. In a resource poor setting, it is justifiable to use TSH alone for initial screening, which is satisfactory so long as its limitations are appreciated. In difficult cases when the suspicion of thyroid dysfunction remains high, a combination of all three tests (TSH, free T3* free T4) will usually avoid misdiagnosis. T3 or T4 estimation alone as an initial screen, however, will miss subclinical thyroid dysfunc-
tion and is not advised. One should be aware of condi-
tions in which TSH alone might be misleading like re- cent treatment of Thyrotoxicosis, Pituitary disease, non- thyroidal illness and thyroid hormone resistance.
Who should be sc*eened for thyroid dysfunction?
We should look for subtle signs of hypothyroidism in all patients, especially among women pre*enting with gen- eralized weakness/menstrual irregularities and screen
them. Mandatory screening in pregnanc* is desirable.
All geriatric patients should be screened upon admis- sion to the hospital. Women ≥ age 50 years who seek medical care should be screened. Women in high risk gr*ups (those with an autoimmune disease or with a strong family history of thyroid disease) should be screened starting at 19 years of age. Biochemical screen- ing for thyroid dysfunction is advocated in all dyslipidemic patients and in patients with unexpected improvement or worsening of lipid profile.
In clinical practice, six different patterns of the thre* main thyroid function tests (T*H, free T3, *ree T4) are seen. We will restrict our discussion to scenarios of hy- pothyroid state.
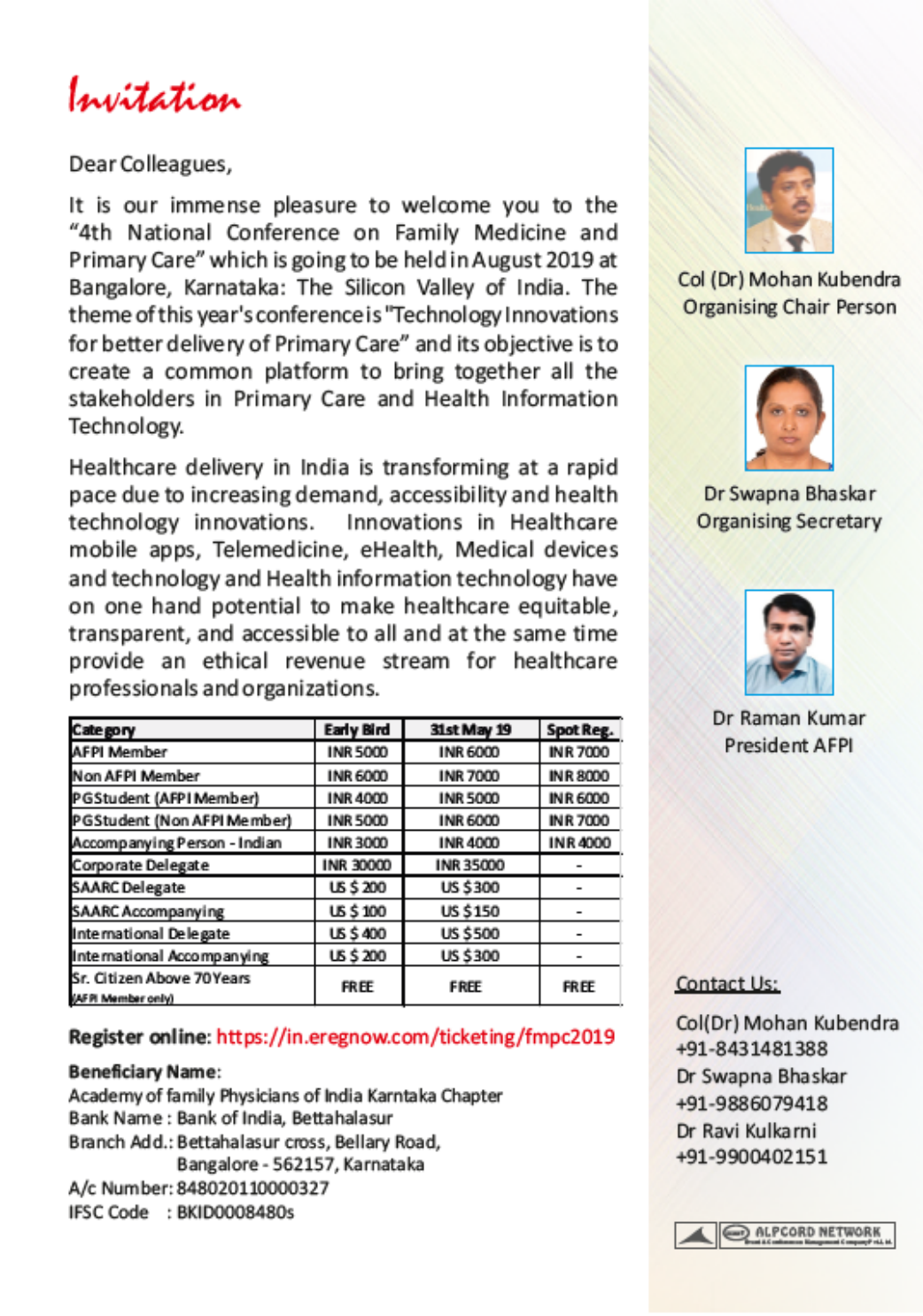
Scenario 1: Raised TSH, normal free T4 or T3
This is the pattern of thyroid dysfunction normally seen with mild thyroid failure, a condition called subclinical hypothyroidism. This is common in the population, af- fecting 5 to10% of all women. It is mostly caused by au- toimmune hypothyroidism that has not *et progressed to severe thyroid impairment. This can also be seen in patients who have undergone radioiodine treatment or thyroidectomy. Thyroid peroxidase antibody (TPOAb) measurement sh*uld be considered when evaluating
5
Gleanings
patients with subclinical hypothyroidism as it helps to define the risk of developing overt hypothyroidism.
Any patient with subclinical hypothyroidism an* a TSH >10mIU/L should be treated. In patients who have a TSH <10mIU/L, treatment should be considered in pregnant women or women planning pregnancy, those with infertility, those with a goiter, or individuals with elevated antithyroid peroxidase antibody levels. A re- cent study favors treatment if prolactin is elevated with menstrual disturbance even if Anti TPO Ab is negative. New clinical data also suggest treatment of subclinical hypothyroidism in those with chronic kidney disease (CKD) irrespective of symptoms or antibodies. It is pru- dent to avoid treatment in patients with subclinical hy- pothyroidism who are older than age 85 years. The aver- age dose of T4 replacement for subclinical hypothyroid- ism in adults is 25mcg (12.5 mcg in adults weighing < 50 Kgs).
Although subclinical autoimmune hypothyroidism is by far the most common cause of this pattern of thyroid function tests, alte*native diagnoses should be consid-
ered under certain circumstances like intermittent T4
th*rapy for hypothyroidism, TSH-receptor defects and use of certain drugs like amiodarone, sertraline, choles- tyramine.
Scenario 2: Low or normal TSH, low free T3 or T4
Low or normal TSH and low free T3 or T4 test results represent a typical pattern in unwell patients with Nonthyroidal Illness,[ the most common combination of
results being a low free T3 with a TSH in the normal
range and recent treatment for hyperthyroidism( when both free T3 and TSH remains suppressed).]?

Non-thyroidal illness(NTI) describes conditions charac- terized by abnormal thyroid function tests encountered in patients with acute or chronic systemic illnesses. A decrease in T3 is the most common finding in these pa- tients while TSH will be normal and *hus provides the best guide of thyroid status. However, in some patients, TSH concentrations may b* suppressed in the acute phase and on recovery TSH concentrations may rise transiently into the hypothyroid range. It is for this rea- son that performing thyroid function tests is not advised for ill patients *nless specifically indicated.
Medication side effects: Certain medications can have the unintended side effect of affecting thyroid fu*ction. The following med*cations have been linked to various forms of *hyroid disease:
-
• Amiodarone (more commonly can lead to hypothy- roidism, but can be associated with some types of hyperthyroidism)
-
• Lithium salts (*ypothyroidism)
-
• Some types of interferon and IL-2 (thyroiditis)
and somatostatin analogs (block TSH, which can
lead to hypothyroidism)
Scenario 3: Raised TSH, low free *4 or T3
This combination of results always indicates primary hypothyroidism. In iodine sufficient areas, almost all cases are due to thyroablative therapy for thyrotoxicosis or if they arise spontaneously, autoimmune thyroiditis manifested as Hashimoto’s disease. Anti thyroperoxi- dase antibodies are said to be present in more than 90% of cases of chronic autoimmune thyroiditis. When thy- roid function tests suggest primary hypothyroidism, but anti-TPO antibodies are not detectable, rarer causes should be considered.
Treatment of Primary Hypothyroidism
With the exception of certain conditions, the treatment of hypoth*roidism requires life-long therapy with syn- thetic T4 Thyroxin. The average dose of T4 replacement in adul*s is approximately 1.6 ug/kg/day for <60 years and 1ug/kg/day for > 60 years (due to reduced metabo- lism of thyroxine). This translates into approximately 100 micrograms per day for an adult weighing 60 Kgs. Loading dose depends upon TSH levels. Start with 25 micrograms or less of replacement hormone, with a gradual increase in the dose based on the TSH levels at
6-week intervals. But if TSH > 20 and you are starting
low dose then up titrat* once in 2 weeks by 12.5 mcg till u reach dose of 1ug/kg and then once in 6 weeks. Once stable, the TSH can be titrated once in 6 months. Over- treating hypothyroidism with excessive thyroid medica- tion is potentially harmful and can cause palpitations, high blood pressure and can also contribute
6

Gleanings
Causes of Overt Hypothyroidism

7
Gleanings
to osteoporosis. Every effort should be made to keep the TSH within the normal range. Substitution therapy with L-thyroxine significantly improves lipid metabolism abnormalities. 4-6 weeks of *hyroxin replacement thera- py is usually needed to co*rect dyslipidemia in overt hypothyroidism.
Thyroxine should be taken in empty stomach early in *he morning. No drug / food intake till 60 mins after consuming thyroxine. Alternatively it can be given at bed time provided 2 hrs have elapsed from last meal. Other medications containing iron or antacids should be avoided, because they interfere with absorption.
Take home messages:
As general physicians, we should be aware of the com- mon pitfalls in the interpretation of Thyroid Function Tests(TFT) and adopt a practical approach in dealing with thyroid dysfunctions.
One should have low clinical threshold in asking for op- portunistic and routine TSH screening of desirous/
affordable patients specially among female. [reword]
In a resourse poor setting it is justifiable to use TSH alone for initi** screening, which is satisfactory so long as its limitations are appreciated.
Always ask for Thyroid tests from a reputed lab.
Certain medications like Amiadarone, glucocorticoids, dopamine agonists, and somatostatin
analogs can have the unintended side effect of affecting
thyroid function.
Performing thyroid function tests i* not advised for ill patients unless specifically indicated due to possibility of abnormal TFTs encountered in patients with acute or chronic systemic illnesses, a condition called Non- Thyroidal Illness. (NTI)
Clinically euthyroid with elevated TSH need not be
treated but periodic monitoring is desirable if TSH is <10 mcg. Persistent subclinical hypothyroidism with TSH more than 10mcg will be treated. Will treat even if TSH is between 5-10 when Anti TPO Ab is positive.
All symptomatic hypothyroidism with thyromegaly needs evaluation in the form of TPO Ab, thyroid scan based on which an uptake study. Start with a low dose Thyroxine and titrate the dose
based on TSH levels at least once in 6 months
Thyroxine should be *aken in empty stomach early in the morning. No drug / food intake till 60 mins after consuming thyroxine. Alternatively, it can be given at bed time provided 2 hrs. have elapsed from l*st meal.

Drawn from the Friday night [19/11/2017] web-based discussion
Expert- Dr D.M. Mahesh, Consultant Endocrinolo- gist, Columbia Asia Hospital
Moderator- Col(*r) Mohan Kubendra, Consultant Family Medicine
*
Case Reports
Case Report 1
A Case of Disseminated Tuberculosis with Infec- tious Mononucleosis
Abstract
A case of prolonged fever which was initially thought to be due to Infectious Mononu*leosis (IM) which later proved to be due to disseminated tuberculosis is present-
ed. Test for IM was done first which was positive. This
may have delayed the much more serious diagnosis of Disseminated Tuberculosis.
Introduction
It is uncommon for two febrile illnesses to occur together or one leading to other. This is especially so in family medical practice. In the US where the first illness (IM) was detected, the doctor may be excused for reassuring
the patient as one would no* think of TB specially so be-
cause TB is a rare illness in the US. It is only after the pa- tient returned to India that the possibility of IM trigger- ing TB or TB concurrently being present was thought off and investigated. A net s*arch with words Tuberculosis and Infectious Mononucleosis produced no results. The authors/reporters fe*l that this may be the first such case that is being reported.
Case Report
Deepak, a 26-year-old software engineer working in the USA for the past two and a half years presented with a history of fever of 5 weeks duration, weight loss of 8kgs and cough with expectoration of a week’s duration on Ju- ly 26, 2017
A detailed history of the present illness revealed that his fever b*gan intermittently and later became continuous
with chills and temperature ranging from 103 to 104F
along with severe sweating. No history of pain abdomen, yellow eyes or urine. The cough was mild and there was no blood in the sputum, there was severe loss of appetite and loss of weight. He had consulted the designated phy- sician in the US on June 28,17, who had ord*red routine tests which included hemogram, blood culture, Chest X- ray, Paul Bunnel test for Infectious Mononucleosis (IM) IgG and IgM for Infectious mononucleosis came back as
positive on July 7, 2017) Patient was assured that all will
be well in the course of time, advised bed rest and symp- tomatic treatment to keep the fever and body aches down. After ten days, as the symptoms did not abate, the doctor was contacted who reassured the patient that it takes 6 to 8 weeks for the symptoms to recede and there is no cause to worry.

As the fever continued to remain high, with severe loss of appetite, with no support system existing in the US, the patient decided to get back to Bangalore and came to see me on July 26, 2017.
Nothing relevant in his personal, family and past history.
On Examination
Well built, weighing 75KGs, 5.10” tall (BMI 24), looking ill and sick, temperature of 103, pulse 140 per minute, regular, BP 120/80, profusely sweating, no evidence of jaundice, anaemia, dyspnoea, oedema Cervical lymph glands. Both sides enlarged more on left side, mildly ten- der, not hard. A few axillary lymph glands felt non- tender. Inguinal lymph glands not enlarged. Skin normal. All other systems were norma* on examination.
Investigations done in the US
-
• Blood ESR 18 mm/hr
-
• Blood Culture & Sensitivity. No growth after 5 days
-
• X-ray Chest PA view and Lateral view. No evidence of active pulmonary disease
-
• Epstein Barr Antibody Test. IgM Positive
Following tests were ordered here
(Only relevant investigations are mentioned)
-
• Hb% 12.2 WBC. TC 7800 N80 L11 Mono 8. ESR 67 mm/hr
-
• Urine routine: Normal. Blood Urea: 17.8 mg. HIV Negative
-
• S. Creatinine 0.96 mg. Widal test negative. Typhi dot IgM negative
-
• LFT SGOT 74 SGPT 137 GGTP 441.
-
• Sputum for AFB negative x 3 days
-
• Sputum for GenExpert Negative
-
• Blood Culture & Sensitivity. No growth after one
w*ek
-
• Chest X-Ray Pa view. Impression: Features of medi- astinal adenopathy with pulmonary parenchymal mil- itary mottling. To rule out Koch’s.
-
• CT Scan of Thorax. Impression: Multiple Miliary nodules throughout the lung fields. Conglomerate and necrotic mediastinal lymph nodes. Left level II* and level IV lymph nodes Overall features are sugges- tive of Tuberculosis. CT Thor*x showing mottling of both lung fiel*s, goes in favour of Miliary Tuberculo- sis.
9
Case Reports
-
• To confirm and clinch the diagnosis, Excision Biopsy of left cervical lymph glands was done. Biopsy report. Wide areas of caseation necrosis rimmed by epitheli- oid cells and lymphocytes* Ziehl-Neelsen stain shows occasional acid-fast bacilli. Imp*ession: Tu- *erculous Lymphadenitis – Left supra*lavicular lymph node.
-
• Gene Expert MTB/RIF of supra clavicular cervical
lymph node. Result: Mycobacterium tuberculosis:
MTB D*t*cted low Rifampicin Resistance – *ot de- tected
With the above results, a diagnosis of disseminated Tu- berculosis was made and the patient was started on standard four drugs anti tuberculosis treatment.
After 10 days of treatment with 4 drug anti tuberculosis
*reatment, patients fever came down, sweating ceased,
appetite improved, and he ga*ned a Kg and half weight. B*t, it took four months of therapy for the fever to return to normal
At the time of reporting, six months into treatment the patient is asymptomatic and has reached his old weight.
Discussion
This patient threw up many diagnostic challenges, not the
least be*ng te*ting positive for Infectious Mononucleosis, which led the doctor to reassure the patient that all will be well despite more than two weeks of fever. Normally IM settles dow* and patients become fever free in ten days to fifteen days, though asthenia continues for weeks. As the fever kept going up unabat*d with other constitutional signs and symptoms, it became necessary to consider oth- er diagnostic possibilities.
Given the presence of fever with adenopathy and cough, the following possibilities were thought off. Though tu- berculosis was still high on the list, Lymphoma, Sarcoido- sis, Typhoid fever, HIV wi*h opportunistic infection were considered. The investigations done, ultimately clinched the diagnosis of disseminated tuberculosis,
Could this have been a case of disseminated TB from the inception and the positive IgM for IM was incidental and the patie*t did not have overt IM at all? The matter was researched and it was found that most people acquire EBV which causes IM when they are young, and it often remains as a persisten* and latent infection with both IgG and IgM often being positive. It is unlikely that an acute
10

episode of IM triggered this TB, as it would be many weeks after the EBV infection that TB would develop, giv- en the slow replication time of the tubercle bacillus Clini- cians should be a*are of the possibility of two infections simultaneously occurring or one facilitating the occur- rence of the other
Conclusion
A Case of Disseminated Tuberculosis with IM is present- ed. This caused initially some diagnostic dilemma.
Dr. H. S. Mruthyunjaya dochsm@yahoo.com
Reporter acknowledges inputs from Drs B.C. Rao, Rama- krishna Prasad and Dr. Peter Veldkamp (University of Pittsburgh)
Case report 2
A blessing for one but curse for another: A case of OCP induced Cerebral Venous Thrombosis.
Abstract
Cerebral Venous Thrombosis (CVT) is a rare and poten- tially life-threatening condition where ther* is clotting of the cerebral venous system, commonly seen in young population. Oral Contraceptive Pills (OCP) are one of the major risk factors for CVT in females. We are presenting the case of a teenager who was prescribed OCPs to control her menorrhag*a and polycystic ova*ian disease (PCOD) but developed CVT within three weeks of its usage.
Keywords. Oral contraceptive pills, cerebral venous thrombosis, PCOD.
Case Report
A 16-year-old girl was brought to the ER at midnight with generalized weakness and headache of 7 days, which had aggravated since the last evening. She had menorrhagi* for 25 days one and a half months ago and was diagnosed to have PCOD in her pelvic scan, for which she was start- ed on OCPs by her gynecologist. Her bleeding had stopped since few days and she was continuing her pills with iron supplements. Her family physician noticed that the patient was unduly tired, severely anemic, restless and referred her for a detailed workup.
Case Reports
Her headache was initially in the left frontotemporal re- gion, but slowly progressed to right side also and had in- creased in severity with nonbilious vomiting, photopho- bia and prostration since past 24 hours, although not as- sociated with nausea or fever. She also had dyspnea on exertion – Mmsa grade 3 for the past few days. The pa- tient had a past history of idi*pathic hypothyroidism for which she was on hormone replacement [thyroxine,50mcg]. No other relevant pa*t history was obtained.
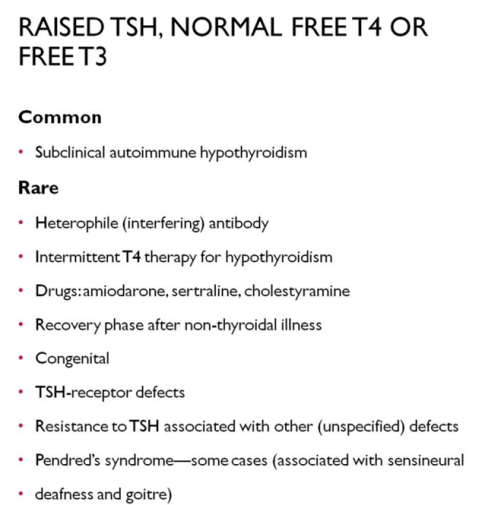
On examination her vitals were stable, but she looked to be in distress, answerin* incoherently and crying due to pain. There was no neck rigidity or any other neurological deficits. She was severely pale an* had a short systolic flow murmur in the aortic area. There were no other sig- nificant physical findings. She was admitted with a diag- nosis of severe anemia, PCOD, and encephalitis and start- ed on IV paracetamol for pain relief, mebendazole, and ondansetron. CT brain was ordered along with hemo- gram, iron profile, Renal, liver and thyroid function tests. As she was being shifted for CT, the patient developed tonic seizures with post ictal drowsiness and was immedi- ately treated with IV levetiracetam and shifted to Inten- sive care unit (ICU) for further intensive observation. Her blood investigations showed HB of 5.5gm, other cell counts RFT, LFT and TSH were nor*al, But CT brain showed CVT (figure 1). She was started on Low Molecular Weight Heparin (LMWH), continued with antiepileptics and ot*er symptomatic care and a neurology opinion was sought. MR venogram was done which confirmed the CVT (figure 2). Prothrombin Time, INR and ANA profile were normal on initial testing and she was starte* on a*itrom from 3 rd day with regular monitoring of INR till it reached 2.2. Her headache resolved in 3 days, sensorium returned to full normalcy but she started to have bleeding PV on day 4 for which a gynecologist’s opinion was taken and started on tranexamic acid to control bleeding. Pa- tient was also transfused 3 pints of packed cells during the stay to correct the anemia and was discharged on day7 with anticoagulants, iron supplements, and antiepi- leptic with advice regarding need for regular PT/INR
monitoring. Further workup for other causes of CVT like
coagulation profile, protein C and S, antithrombin 3 etc. were deferred to a later date due to consensus among the treating team of the etiology being the intake of OCPs and initiation of LMWH as an emergency measure.
11


Case Reports
Discussion
The incidence of CVT is estimated to be around 3 - 4 cases per one million people and most commonly o*curs be- tween the ages o* 20 - 40 years with a mean age of 38.7 years [1, 2,3]. Due to the variability of presenting symptoms, misdiagnosis or delay in treatment is common. Therefore, it is important for clinicians to consider CVT when evalu- ating patients at increased risk of thrombosis. The cause of thrombosis can remain uncertain in 20-30%cases in spite of detailed evaluation (4) . The various risk factors for CVT includes pregnancy, *CPs, hyperhomocystenemia, CNS infections, autoimmune diseases, trauma, malignan- cy, infections, thrombophilia, conditions which may cause tissue damage and stasis, dehydration, and congenital or acquired abnormalities of the hemostatic system (5,6,7,8,) . The most common clinical features are headache, papilledema, seizures, sen*orimotor deficits, decreased level of consciousness and hemorrhage. Severe presenta- tions incl*de focal findings, s*ch as hemipares*s or apha- sia due to bilateral or unilateral edema and hemorrhagic infarction of the basal ganglia and thalami (9). CVT also accounts for 0.5% of strokes in young. Significant disabil- ity le*ding to dependency has been reported in about 5– 10% of patients, and mortality rates range from 3 to 15%
(7) .
CVT is three times more prevalent in women, especially in those taking oral contraceptive pills (OCPs) (10,11) . A recent metanalysis found a 7.59 time increase in inci- dence of CVT among women on OCPs compared to those without (12) but did not find the answer on the durati*n and forms of pills which caused the same, whereas many studies suggest increased chances in patients taking third generation OCPs (5,13,14,15.) . An Iranian study found a link between use of even short course of OCPs and incidence
of CVT in women (16) . A similar meta-an*lysis showed use
of OCP along with assoc*ated other risk factors increased the odds of CVT by up to 22-fold. (17)
Protein C resistance secondary to factor 5 Leiden defi- ciency or prothrombin gene mutation is thought to be the causative factor for OCP induced CVT. The complex changes of the hemostatic system in OCP users *nclude s*imulated procoagulation, inhibi*ed anticoagulation and
elevated f*brinolytic activity. Increased fibrinolytic activi-
ty is caused by elevat*d plasminogen level and a higher tissu* plasminogen activator (tPA) activity. The plasmin- ogen activator inhibitor I (PAI – I) antigen and activity also decrease in OCP users and so does increased clotting acti*ity mediated by platelet activation. Procoagulation
12

activity caused by increased activity of coagulation factors VII, X and fibrinogen is a common finding in almost all preparations of OCPs. Hence the increased incidence could be multifactorial. The World Health Organization recommends avoiding using OCPs in women who have thrombogenic mutations, who smoke, are older than 35 years of age, and who have given birth 21 days prior to starting an OCP to prevent thromboembolic complica-
tions (18.19)
Diagnosis *s confirmed with neuroimaging including CT angiography or MR angiography. Treatment consists of heparin, anticoagulation and in some cases thrombolytic therapy. The overall prognosis of CVT is favorable but, further research is needed to outline optimal treatment options including the duration of anticoagulation therapy and the role of thrombolytic therapy to prevent se*ious neurologic deficits. (18)
The largest study of cer*bral venous sinus thrombosis, the International Study on Cerebral Vein and Dural Thrombosis (ISCVT), was a prospective multicenter ob- servational study of patients with CVT that included 624 adults with CVT to examine the natural history and out- come of disease. The most common presenting symptoms wer* headache, paresis, papilledema, and seiz*re. This study found that most patients present within 4 days of symptom onset; 37.2% with an acute presentation, 55.5% with a sub*cute presentation, and 7.2% with a chronic presentation. Delay in presentation can be attributed to the often-vague presenting signs and symptoms and many a time there is delay in diagnosis even after seeking medical attention. In the study 83.3% of patients were acutely treated with in*ravenous heparin or low molecular weight heparin and at 6 months 79.6% of pa*ients contin- ued to take oral anticoagulation. The thirt*-day mort*lity
rate was 3.4% while 79% of patients experienced com-
plete recovery within six months (20) . Significant disability leading to dependency has been reported in about 5–10% of patients, and mortal*ty rates range from 3 to 15% (21).
Diagnosis in our patient was done with CT and MR veno- gram which confirmed the CVT. Early suspicion and im- mediate use of LMWH and anticoagulation helped in her complete recovery in spite of vague symptoms which were
attributable to severe anemia and /or CNS infection.
Dr. Swapna Bhaskar, *amily Physician Dr. A.R. Bhat Neurologist
Dr. B.C.Rao Family Physician
12 Medical tests to avoid
-
1. Avoid Inducing Labor or C-Section Before 39 Weeks Delivery prior to 39 weeks is associated with increased
risk of learning disabilities, respiratory problems and oth-
er potential risks. While sometimes induction prior to 39 weeks is medically necessary, the recommendatio* is *lear that simply having a mature fetal lung test, in the absence of appropriate clinical criteria, is not an indica- tion for delivery. (American College of Obstetricians and Gynecologists; American Academy of Family Physicians)
-
2. Avoid Routine Annual Pap Tests
In average-risk women, routine annual Pap tests (cervical
cytology screenings) offer no advantage. (American Col- lege of Obstetricians and Gynecologists)
-
3. Avoid CT Scans To Evaluate Minor Head Injuries Approximately 50 percent of children who visit hospital emergency departments with head injuries are given a CT scan. CT scanning is associated with radiation exposure that may escalate future cancer risk. CT technology ex-
poses patients to approximately 100 times the radiation
of a standard chest X-ray which itself increas*s the risk of cancer. The recommendation calls for clinical observation prior to making a decision about needing a CT. (American Academy of Pediatrics)
-
4. Avoid Stress Te*ts Using Echocardiographic Images The recommend*tion states that there *s very little infor- mation on the benefit of using stress echocardiography in asymptomatic individua*s for the purposes of cardiovas- cular risk assessment, as a stand-alone test or in addition to conventional risk factors. (American Society of Echo- cardiography)
-
5. Avoid Prescribing Type 2 Diabetes Medication To Achieve Tight Glycemic Control
The recommendation states that there is no evidence that using medicine to tightly control blood sugar in older dia- betics is *eneficial. In fact, using medications to strictly achieve low blood sugar levels is associated with harms, including higher *ortality rates. (American Geriatrics Society) -
6. Avoid EEGs (electroencephalography) o* Patients with Recurrent Headaches.
Recurrent headache is the most common pain problem, affecting *p to 20 percent of people. The recommenda- tion states that EEG has no advantage over clinical evalu- ation in diagnosing headache, does not improve out- comes, and increases costs. (American Academy of Neu- rology)
13

-
7. Avoid Routinely Treating Acid Reflux
Anti-reflux therapy, which is commonly prescribed in adults, has no demonstrated effect in reducing the symp- toms of gastroesophageal reflux disease (GERD) in in-
fants, and there is emerging evidence that it may in fact
be harmful in certain situations. (Society of Hospital Medicine)
-
8. Avoid Lipid Profile Tests
Lipid Profile test checks various parameters of blood, suc* as cholesterol (good or high density lipoprotein as well as bad or low dens*ty lipoprotein) and triglyceride levels. Several scientific papers have proven that people
with high so-called “bad” LDL cholesterol live the longest
and there is now a large number of findings that contra- dict the lipid hypothesis that cholesterol has to be low- ered at all.
-
9. Avoid Mammograms
Mammograms and breast screening have had no impact on breast cancer deaths and have actually been found to increase breast cancer mortality. With toxic radiation, mammogram testing compresses sensitive breast tissue causing pain and possible tissue damage. To make mat- ters worse, the false negati*e and false positive rates of mammography are a troubling 30% and 89% respective- ly. Another concern is that many breast cancers occur below the armpit*; however, mammography completely misses this auxiliary region, viewing only the breast tissue compressed between two plates of glass. Considering these drawbacks, breast thermography should be given closer consideration. Thermography is a non-invasive and non-toxic technique which can detect abnormalities be- fore the onset of a malignancy, and as early as ten years before being recognized by mammography. This makes it much safer and potentially life-*aving health test for women who are unknowingly devel*ping abnormalities,
as it can take several years for a cancerous tumor to de-
velop and be detected by a mammogram.
-
10. Avoid PSA Testing
A PSA blood test looks for prostate-specific antigen, a protein produced by the prostate gland. High levels are supposedly associated with prostate cancer. The problem i* that the association isn’t always correct, and when it is, the prostate cancer isn’t necessarily deadly. Nearly 20 percent of men will be diagnosed with prostate cancer, which sounds scary, but only about 3 percent of all men die from it.
The PSA test usually *eads to overdiagnosis — biopsies and treatment in which the side effects are impotence and incontinence. Moreover, there is so*e evidence which suggests that biopsies and treatment actually aggravate prostate cancer. During a needle biopsy, a tumor may need to be punctured several times to retrieve an amount of tissue that’s adequate enough to be screened. It is be- lieved that this repeated penetration may spread cancer cells into the track formed by the needle, or by spilling cancerous cells directly into the bloodstream or lympathic system.
-
11. Avoid Routine Colorectal Cancer Screening
Colorectal cancer screening often results in unnecessary removal of benign polyps which are of no threat to pa- tients and the risks of their treatment or removal far ex- ceed any benefit. The evidence is insufficient *o assess the benefits and harms of computed tomographic colonogra- phy and fecal DNA testing as screening modalities for colorectal cancer. -
12. Avoid DEXA
Dual energy X-ray absorptiometry (DEXA or DXA) in a
Practice Experience*
Capt. Singh is now 90 plus and lives in London. For twen- ty odd years he lived here in Bangalore, close to where I live and practice. This was after he retired from Air India
as a senior pilot. This entitled him benefits of unlimited
first-class travel and he spent many months in a year go- ing to the UK and USA where his extended family lived. Then, he had separated from his wife and lived alone, though he kept in touch with his wife and children and frequently visited and stayed with them.
He loved his dri*k and often suffered bouts of upper ab- dominal pain which more often than not he treated him-
self. Occasionally, however, he sought help from the des-
ignated Air India doctor *ho prescribed more or less the same drugs that he himself was taking.
In one of these episodes he came to see me as neither his self-medication nor his doctor’s prescriptio* seemed to work despite him trying these for several days. I found him *n some pain and found the*e was some guarding and tenderness below the right rib cage. Going by his history of repeated episodes of similar pain and clinical findings the diagnosis of gallbladder stone with a possibility of early cholecystitis was not difficult to make. I sent him for an ultrasound study which confirmed the diagnosis.
As the condition needed urgent *ttention, I asked him *o
14

technique developed in the 1980s that measures, among many things, bone mineral density. The scans can deter- mine bone strength and signs of osteopenia, a possible precursor to osteoporosis. Limitations abound, though. Measurements vary from scan to scan of the same person, as well as from machine to machine. DEXA doesn’t cap- ture the collagen-to-mineral ratio, which is more predic- tive of bone strength than just mineral density. And high- er bone mineral density doesn’t necessarily mean strong- er bones, for someone with more bone mass will have more minerals but could have weaker bones.
Dr. S. R. Jayaprakash srjpgm@gmail.com
Further reading:
Choosing Wisely. http://www.choosingwisely.org/wp- content/uploads/2015/04/Final-Choosing-Wisely-Survey -Report.pdf
see the surgical gastroenterologist friend of mine and fixed an appointment for the same evening.
I got a call from that Doctor that evening, informing me
that Capt. Singh has not turned up to keep the appoint- ment.
The matters thus stood for three days.
He came to see me after three days and told me the story. After seeing me he went to his Air India doctor to get a referral letter. That doctor, though agreeing with my diag-
nosis and the urgency, referred him to another doctor in
another corporate hospital. He was admit*ed and operat- ed upon and his gallbladder with the stone was removed lap*rascopically. He was put on antibiotics and was asked to stay for three days for observation and for taking IV antibiotics.
He was supposed to be in the hospital and he is here in my clinic as though nothing has happened. I asked him. He said, ‘’I was pain free and felt good and was feeling very hungry, the nurse refused to give me food and was giving me only fruit juice, I got angry and called the doc- tor and asked him to discharge me’’!
He had come out of the hospital the previous night against advi*e, and had eaten a hearty dinner and break- fast this morning.
I was speechless.
Before he took leave, he said,” you may like to look at this” and took out of his pocket a well-polished half an inch diameter stone which was sitting in his gallbladder.
Some months later I went to his home as his US based sister was down with fever and too ill to see me in the clinic. After the formalities of th* visit was over, he drew my attention to his display case, there sitting on the man- tlepiece was this gall bladder stone proudly mounted on a small metal pedestal.
I am pretty sure that *t must have made many an evening party come alive with its story and my part in it!
Dr. B. C. Rao
In the cause of service
Medical community has a number of individuals who ren- der service driven by a desire to serve persons who cannot afford or don’t have access to, preventive and curativ* health care. Often their work goes unnoticed in this era of biased reporting that highlights some rare surgery or a VIP getting world class treatment in some tertiary care
corporate hospital.
It’s our privilege to introduce a doctor couple, Nithyanand and his wife, Sujatha, bo*h general practi- tioners, p*acticing in Anjananagar, a suburb of Bangalore city. Many years ago, Dr Nithyanand met Dr Ram Reddy who had spent his entire career in rural medical service and was well aware of the many problems faced by the rural population. In one of his talks with Nithyanand, Dr
Reddy discussed about the dire need of deworming the
rural population. That was in the year 1999 and this made them begin distributing Albendazole tablets to people including women and children living in villages they visit- ed once a month. The deworming was done once in six months. For the first three years they concentrated on seven vil*ages around Muddenhalli. During these visits they noticed many pregnant and lactating women suffer- ing from severe anemia and protein deficiency. This made
them to distribute in addition to Albendazole, ferrous sul-
phate 300 mgs tablets and homemade Sai protein pow- der. Sai protein powder is a homemade preparation. The ingredients are ragi, wheat, par boiled rice, green gram, groundnut, jowar and roasted chenna dhal which are all fried and ground into a powder. This powder is made into a porridge and taken by the mothers. They also started

giving calcium tablets.
In the beginning, they went door to door to distribute the albendazole tablets. They made the villagers swallow the tablets in front of them. What began *n the 7 villages gradually spread to cover all the 63 *illages that come under Muddenhalli PHC. They set up distribut*on centers at 18 different strategic locations to cover these villages and now there is no longer any need for them to actually go to the individual homes.
Concurrently, they also educated pregnant women and lac*ating mothers about the importance of health and hy- giene. Many myths about dietary habits in lactating mothers were also addressed. Pregnant and lactating mothers now look forward to the*r visits and there is a noticeable improvement in general health condition. At post-delivery, because their hemoglobin levels are good, these women get selected for family planning operations.
They get a lot of help from vo*unteers, Asha workers and the staff at the PH* at Muddenhalli and the sub centers attached to the PHC. Dr Muniyappa, who is at present manages the PHC is of great help in their work.
What starte* as a dream and wish of this doctor couple has now expanded to form a mission called Divine mother and child health program. Today the program covers 22 PHCs of Chikballapur district with the support of more than 30 d*ctors and 50 volunteers each month. Program intends to improve the q*ality of maternal and child health services within the government health system.
Program is improving each month as m*re number of
individuals and organizations who volunteer is increas- ing.
Drs Nithyanand and Sujatha can be contacted at dr.stnityananda@gmail.com a*d 919845558940
Our newsletter *s open to such stories and read- ers are welcome to write to us if they come across such doctors and their work
15

MASALA
Jump Cure
Mr A has been my patie*t for some years now. He was someone high u* during his working life and sadly he makes it a point for others to know this and I being no exception. More often than not, he begins the consult
with the opening rema*k,’ when I was----, designed to put
me off.
He h*d another unwelcome attitude, that is to praise or attribute to s*me other treatment or procedure o*her than what I had recommended being responsible for his cure. Once or twice I had even asked him, why then come here to consult with me? His excuse was that I give mini- mum medication! Irrelevant explanation.
Some years back he underwent TURP after consulting many doctors and lay persons who had undergone the procedure including a trial of homeopathy. He remained
free from symptoms till recently when he developed symptoms of UTI. Pending investigation, he was advised to begin a tentative antibiotic. He phoned that evening complaining of very frequent urination and a struggle to initiate a flow. He also said he is drinking lots *f wat*r. I told him to limit his water *ntake and await the reports. He came next morning with his urine report which
showed pl*nty of pus cells and 20 to 30 red cells, con-
firming the diagnosis of UTI.
I asked him about the hesitancy to pass urine that he was having the previous day.
He said,’’ yo* know doc, the yoga teacher who comes home, tol* me to jump up and down, which I did and be- lieve me it worked like magic’’
There, he was true to his character. No credit to his doc- tor and his medication


www.afpikarnataka.in
This place is open for advertisements. To place an advertisement, please contact our editorial team.
16