
President’s Letter

While growing professional and social commitments kept me away from active participation in our closed social media discussions, this column gives me an opportunity to periodically reflect upon our achievements and shortcomings.
It’s more than a year since we started this Newsletter and have brought out five editions so far. The outcomes of any constructive efforts are highly dependent on the ensuing input, critique and conviction by the team. Needless to say, that the editorial team has put in their heart and soul in making this newsletter not just a reflective document but has set standards to ensure the objectivity, credibility, and quality of the published material on the newsletter.
I must ad*it that I am a bit disappointed with the poor subscription and suboptimal contribut*ons from the readers. The core mission of this newsletter is to act as an instrument for reflections of your practice experience and publication of quality articles of importance to primary care physicians. It’s my earnest request to all reade*s to actively contribute in complementing the efforts of the editorial team.
Looking back at the last quarter- in r*sponse to a joint initiative by the State RNTCP unit and National Tuberculosis Institute (NTI) to augment active case finding and notification of newly detected TB cases AFPI organized a workshop to sensitize Private practitioners. It will be our endeavor to plan our future activities which are aligned with Government programs and policies. In another notable new collaboration with Shifa Hospital ‘Family Medicine update’ was conducted on 1 st of July with interesting sessions on topics of interest to GPs.
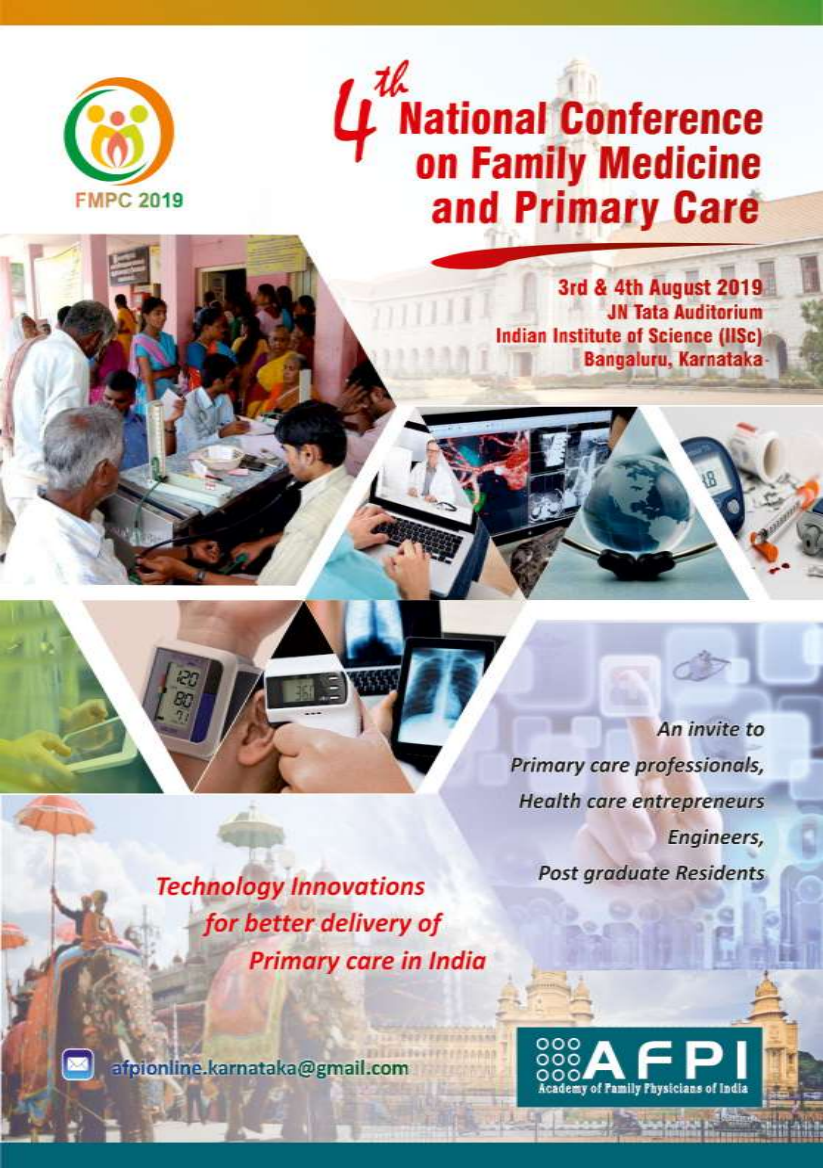
Preparations for FMPC-2019 has picked up pace with a core committee meeting and formation of Organizing committee on the 3 rd of June. We look forward to all our readers taking an active par* in promotion of this event to be held at Bangalore from 2 nd to 4 th of August 2019.
Last quarter has been quite significant for AFPI at the national level. WONCA world Rural Health Conference(WRHC-2018) has been a huge success which compelled the policy makers and other stakeholders to take note of the mission and the *ork of the academy. The emergence of some highly energetic young leaders of Family Medicine has been a big positive of this event. In another significant development a Public Interest Litigation (PIL) filed by AFPI was admitted in the Supreme court of India. The c*urt in its hearing has directed the academy to approach the policy makers for recognizing Family medicine as a specialty of primary care in government establishments. The acknowledgment of the need for strengthening primary care by highest judiciary of the country can be seen as an achievement by itself and should motivate us to continue our efforts for the development of Family medicine both at the state and national level.
AFPI KARNATAKA
Newsle*ter Volume 2/Issue 2
President
Col (Dr.) Mohan Kubendra mohankubendra@gmail.com
Secretary
Dr. Bhaskara Puttarajanna drbhaskarap@gmail.com
Vice President
Dr. Ramakrishna Prasad dr.rk.prasad@gmail.com
Treasurer
Dr. Ravikumar Kulkarni ravikumarkulkarni@yahoo.com
Scientific Chair
Dr. Jaya Bajaj jay*bajaj@gmail.com
Editorial team
Dr. B. C. Rao badakere.rao@gmail.com
Dr. Roshni Jhan Ganguly roshnijhan@hotmail.com
Dr. Ramakrishna Prasad dr.rk.prasad@gmail.com
Call for action- For a long time we have been contemplating engag*ng the young medical students in our activities. A medical student wing of the state chapter will be created within the next few weeks time to invite final year MBBS students for participating in the activities of the academy to understand the concept of Family Medicine and scope of family practice as a career prospect.
Recent developments of growing despair against our profession makes one feel that medical profession is in cross roads. It may not be true but the road is not smooth as well and it is the responsibility of the medical professionals to have the road laid smooth. Nobility is the hallmark of this profession and it is you, who can give the nobili*y to this profession through ethical practice for only ethical practice can redeem the image of the profession.
Once again my sincere thanks to the editorial of this newsletter for creating this platform of sharing knowledge and ideas. I look forw*rd to receiving your input or suggestions to strengthen the mission of thi* piece of diligent effort.
Col (Dr.) Mohan Kubendra
Editorial Note
Doctors working in this country are a worried and unhappy lot. Th*y are under tremendous pressure. Pe*ple’s expectation of cure for all ailments and the inability of doctors to come up to this expectation is resulting in all sorts of mistrust leading to abuse of doctors. On the one hand the societal perception of doctors as greedy exploiters has led to attitudinal changes in the way the doctor sees the patient [defensive medicine], on the other hand i*dustry driven health care where profit is the primary motive has led to doctors being assessed by the revenue they generate and not entirely by their competence.
Hospitals are not factories. These are institutions where human beings in distress are handled. It is agreed that hospitals too need to be profitable *o survive but there needs to be a different kind of approach to patient management keeping in mind the interests of patients, treating doctors and the owners of the hospital. Many hospitals suffer because of keeping the owners interest as the sole priority and because of this, the major sufferers are the ethical doctors working in these hospitals.
A situation has arisen in many institutions, which makes an ethical doctor either to compromise his principles or leave. How many doctors can take the second option and quit? Inevitably those who stay accept the unethical ways and survive and *ive under considerable stress, caused by both the patient population and the management of the hospital.
Family medical practitioners, working in the community are spared from this ongoing turmoil, to a great extent, thanks entirely to the trust and relationship between the patient and doctor. Most illnesses occur in the community and are being managed by community-based doctors, and these are mostly family physicians. Over the past three decades the number of young doctors taking to family medicine as a career choice has greatly come down. One way of reducing the conflict as discussed above is for doctors to promote more effective and transparent communication between doctors and patients that builds conf*dence and trust. In the present scenario, where institutionalised medicare suffers from the many ills,some of which is lised above, family medical practice which is relatively free from these pressures, is a very good career option.
This issue of the newletter, besides its regular sections, has a feature practice management article by Dr. Devashish Saini on how much to charge for consultations. It also has a draft of a young primary care physicians conference, Technology-driven Primary Care – towards Universal Health Coverage” being planned during FMPC 2019. Your engagement and feedback is sought and will be taken into account to shape th*s meeting.
AFPI-NEWS
WHRC 2018 – A Report by Dr. Roshni Jhan Ganguly
More than a thousand delegates from 40 countries participated in the 15th WONCA world rural health conference which took place in New Delhi from 26-29th April, 2018 at the India Habitat Centre. The conference was organized by the Academy of Family Physicians of India in association with WoRSA - WONCA Rural South Asia. Under the theme “Healing the Heart of Healthcare - Leaving No one behind”, this event demonstrated exemplary team work to bring rural healthcare on the global platform.
The inaugura* ceremony was gr*ced by our Vice President Mr. Venkaiah Naidu and *he Honorable Minister for Health and Family Welfare, Government of India, Mr. Ashw*ni Kumar Choubey. The Mission Direction of the Indian National Health Mission (NHM), Mr. Manoj Jhalani, delivered the inaugural keynote address. This event was supported by NHM, Government of India. P*of John Wynn-Jones, Chair of the WONCA Working Party on Rural Practice, delivered the annual John MacLeod Oration. It was indeed encouraging to receive a message from our Prime Minister Shri Narendra Modi where he mentioned the pivotal role of rural healthcare to achieve Healthcare for all.
The Health Minister of De*hi, Mr. Satendra Jain took time off his busy schedule and glorified the healthcare leadership award ceremony on 27 April 2018. Awards were presented to distinguished health care leaders (and well known Rural WONCA identities) for their exemplary service in rural areas.
The most memorable part of this conference was the participation of medical students. The Medical Student Association of India (MSAI)/ IFMSA and JDN (Junior Doctor Network) of the Indian medical association not only actively participated but also shouldered respons*bility in organizing this conference.
Must mention here that an extensive scientific program with 13 keynote speakers, 250 oral presentations 85 e- posters, 60 workshops, 26 Ideathon presentations, 20 panel discussions and 10 symposia spread over eight parallel meeting rooms ran over four days and kept the delegates engaged though out.
Some of the landmark events that took place during the conference were:
-
1) FISFA: International Short Film and Arts Festival: The first in its kind in association with WHRC 2018 showcasing films broadly themed on healthcare issues and attended by film/media professionals, student/ amateur film makers and doctors/ medicos.
-
2) National Consultation of strengthening rural healthcare: Niti Ayog – The policy commission the highest policy making body in India co-hosted a national consultation on strengthening rural healthcare in India, during this conference.
-
3) Delhi Declaration: Delhi Declaration was adopted during the closing ceremony which revisited the Alma Ata Declaration. The aim to achieve a highest possible level of health for the communities we serve, with the goal of “Health for All Rural People.”.
-
4) Sojourn: Pre and Post conference exchange programs were conducted to observe delivery of healthcare i* rural and remote areas.
-
5) Project Setu: An ongoing initiative with the aim of bridging the gap between urban and rural divide.
-
6) Rural Café: Members of Rural Seeds organized a popula* “rural café” during WRHC 2018 which was streamed live.
This conference will be remembered for the involvement of top policy makers, key stakeholders, important health institutions, various medical universities and delegates spanning the whole medical fraternity.


TB UPDATE AND NOTIFICATION - 2018
AFPI Karnataka chapter in collaboration with District TB Office authorities organized a workshop on 23 rd June between 1:30 – 3:30PM to sensitize the private practitioners to facilitate the government agencies in augmenting case finding. Nearly 65-70 practitioners attended the workshop in Jayachamarajendra auditorium at NTI premises. The event attained great importance as it was decided by DTO,(URBAN COMMISSIONER) and other stakeholders to execute IPC 269 & 270 which mandates notification of TB cases. Necessary action would be taken if this was not abided by private practitioners and the KPMEA license would be cancelled. Registrations of individual clinics were done and HEID number was given o* the spot by district T* officers. Notification of TB cases via NIKSHAY app was also demonstrated live. Doctors received Rs 500/- incentive and certification of participation for attending workshop. This was indeed an important step towards joining hands in large numbers to end Tuberculosis. Dr. Somashekhar, Director NTI deserves special mention fo* his proactive and helpful nature. A big thank you to Drs. Mohan, Sowmya and Gowri for taking this initiative and executing it !

Family Medicine Upd*te – Shifa Hospital
In a new coll*boration for AFPI, ‘Family Medicine update' for General Practitioners w*s held at Shifa hospital on 1st July 2018. Topics were thoughtfully selected to meet the needs of Family Practitioners and generated very interesting and Interactive deliberat*ons. It was attended by over 70 delegates.

Gleanings Shingles vaccine- ZOSTAVAX and SHINGRIX
Approximately 25% of people suffer herpes zoster during their lifetime. The most debilitating complication of herpes zoster is post-herpetic neuralgia. Both the incidence and the duration of post herpetic neuralgia are directly related to increasing age. The elderly can be vaccinated with zoster vaccine, which is the same vaccine as varicella vaccine but with a much higher level of vaccine virus. T*e zoster vaccine is not 100% effective in preventing reactivation as herpes *oster. However, cases of herpes zoster and post-herpetic neuralgia after vaccination are less frequent and less morbid than those who had not received the vaccine. The zoster vaccine prevented post-*erpetic neuralgia to a greater extent among the age 70 or more y*ars. People over 60 should receive one dose of zoster vacci*e regardless of previous history of chickenpox or herpes zoster.
ZOST*VAX
The live att*nuated Zoster (Oka/ Merck) vaccine (ZOSTAVAX) for adults can boost host immunity to VZV. It contains the same virus strain as the varicella vaccine for children, but is 14.4 times more potent (1,350 pla*ue- forming units [PFU] vs. 19,400 PFU).
ZOSTAVAX i* *pproved by the US Food and Drug Administration for prevention of HZ (shingles* in individuals ≥50 years, supported by the results of the ZOSTAVAX Efficacy and Safety T*ial (ZEST) and Shingles Prevention Study (SPS). In ZEST, ZOSTAVAX significantly reduced the risk of developing z*ster by 69.8% in comparison to placebo and increased th* VZV-specific antibody geometric mean titers (GMT) by 2.3 fold at 6 weeks post-vaccination in a random 10% subcohort. In SPS, ZOSTAVAX significantly reduced the risk of developing HZ, the bu*den of illness, and PHN by 5*.3*, 61.1%, and 66.5%, respectively, compared to placebo. Vaccine efficacy for the prevention of HZ declined with increasing age.
Except for the increased risk of injection-site adverse ev*nts (AEs), the vaccine was considered safe in the SPS po*ulation. SPS reported a 1.7-fold (95% confidence interval [CI]: 1.6, 1.8) increase in VZV specific antibody titers at 6 weeks postvaccination. An immunogenicity study conducted on the VZV vaccine showed a comparable 1.6-fold increase *n an*ibody titers at 6 weeks. Further, the increase in VZV-specific antibody titer correlated with vaccine efficacy in another study.16
Zostavax is approved by FDA for people age 50 years and older. However, CDC does not recommend routine use of this vaccine in people age 50 through 59 years. Healthcare providers considering the herpes zoster vaccine for cer*ain persons in age ranges should discuss the risks and b*nefits of vaccination with their patients. Although the vaccine has short-te*m efficacy, there have been no long-term studi*s of vaccine protection in this age group. *n adults vaccinated at age 60 years or older, vaccine efficacy wanes within the first 5 years after vaccination, and protection beyond 5 years is uncertain; therefore, adults receiving the vaccine before age 60 years might not be protected when their risks for herpes zoster and its complications are highest.
Zostavax (zoster vaccine live) is administered subcutaneously as a single dose in the deltoid region. The *accine should not be injected intramuscularly. However, it is not necessary to repeat vaccination if it is administered intramuscularly.
SHRINGIX
A new shingles vaccine called Shingrix was licensed by the U.S. Food and Drug Administration (FDA) in 2017. CDC recommends that healthy adults 50 years and older get two doses of Shingrix, 2 to 6 months apart. Shingrix provides strong protection against shingles and PHN. Shingrix is the preferred vaccine, over Zostavax. Shringix is not available in India.
Approval of Shingrix is based on a comprehensive Phase III clinical trial program evaluating its efficacy, safety and immunogenicity in more than 38,000 people. In a pooled analysis of these studies, Shingrix demonstrated efficacy against shingles greater than 90% across all age groups, as well as sustained efficacy over a follow-up period of 4 years
Shingrix (recombinant zoster vaccine) should be administered to adults age 50 years and older as a two-dose series (0.5 ml each), 2 to 6 months apart (0, 2-6 months). If more than 6 months have elapsed since the first dose of Shingrix, you should administer the second dose as soon as possible. However, you do not need to restart the vaccine series.If the second dose is given less than 4 weeks after the first dose, the second dose should be considered invalid. A valid second dose should be administered 2 months after the *nvalid dose (minimum acceptable interval is 4 weeks following invalid dose).
Shingrix should be injected intramuscularly in the deltoid region of the upper arm. vaccine administration error and should be avoided
Subcutaneous injection is a
contraindicated in person with active, untreated tuberculosis and in immunocompromised adults such as those with leukemia, l*mphoma, or generalized malignancy and in patients receiving chemotherapy, radiation, and large doses of corticosteroids.
*he most common side effects are pain, redness, and swelling at the injection site, muscle pain, tiredness, headac*e, shivering, fever, and upset stomach
New on Rabies
If rabies immunoglobulin is not available, double dose of the first dose of vaccination may be administered in the foll*wing situations: (i) category III exposure, (ii) patients who are malnourished and patients receiving corticosteroids, anticancer drugs, and antimalarials, and (iii) patients with HIV/AIDS with CD4+ count
<200/mm . If feasible, antibody titers should be monitored and boosters given if titer is less than 0.5 IU/ml.
3
Typhoid vaccine
The available vaccine* for typhoid fever include inac*ivated who*e cell vaccine, live oral Ty21a vaccine, injectable Vi polysaccharide vaccine, and Typhoid conjugate vaccine. The lyophilized oral Ty21a vaccine is available in two formulations: A liquid suspension (in sachets) or enteric coated capsules. The Vi polysaccharide vaccine is a subunit vaccine composed of purified Vi capsular polysaccharide. [7] To improve immunogenicity Vi was conjug*ted to rEPA, a recombinant exoprotein A from Pseudomonas aeruginosa. Vi- rEPA showed higher and longer lasting anti-Vi IgG in adults and children than Vi alone in high endemic areas. Using eith*r rEPA or different carrier proteins, such as diphtheria or tetanus toxoid, recombinant diphtheria toxin (CRM197), the Vi conjugates synthesized was significantly more immunogenic than Vi alone
Primary vaccination with oral Ty21a vaccine consists of 4 capsules, 1 taken every other day. The capsules sh*uld be kept refrigerated (not froze*), and all 4 doses must be taken to achieve maximum efficacy. Each capsule should be t*ken with cool liquid no warmer than 98.6°F (37°C), approximately 1 hour before a m*al and ≥2 hours after a previous meal. This regimen should be completed ≥1 week befor* potential exposure. The vaccine manufacturer recommends that Ty21a not be administered to infants or to children aged <6 years. A booster dose is recommended every 5 years for people who remain at risk.
The Vi vacc*ne is given as a single subcutaneous or intramuscular dose of 0.5 ml, with revaccination every 3 years.
WHO has prequalified the first conjugate vaccine to prevent typhoid fever called Typbar-TCV® developed by Indian pharmaceutical company Bharat Biotech. The vaccine has long-lasting immunity, requires only one
dose and can be given to children as young as 6 months through routine childhood immunization programmes. Other Typhoid vacc*nes are recommen*ed for children over 2 years of age.
One single 0.5 mL dose of Typbar-TCV, injected intramuscularly, offers protection for at least 3 years to adults, children, and infants over 6 months of age. Further studies are needed to determi*e the duration of protection and need for booster doses.
Entire community at risk should be vaccinated during an outbreak. If immunization of the entire community is not possible, individuals aged 2-19 years should be specifically targeted. Ty21a should not be used during pregnancy. Vaccination policy for renal disease patients is same as for normal population. Live oral typhoid is contraindicated in transplant recipient.
|
Brand Name |
Composition |
Company |
Packin |
MRP |
||
|
g |
Rs. |
|||||
|
TYPBAR inj |
Purified Vi capsular polysaccharide of |
BHARAT |
0.5ml |
175.00 |
||
|
salmonella typhi 0.025mg, phenol 1.25mg |
BIOTECH |
|||||
|
TYPBAR inj |
Purified Vi capsular polysaccharide of |
BHARAT |
2.5ml |
525.00 |
||
|
salmonella typhi 0.025mg, phenol 1.25mg |
BIOTECH |
|||||
|
TYPBAR |
Purified Vi capsular polysaccharide of |
BHARAT |
0.5ml |
1800.0 |
||
|
TC* inj |
salm*nella typhi Ty 2 conjuated to tetanus toxoid 0.025mg, phenol 1.25mg |
BIOTECH |
* |
|||
|
TYPHIM VI inj |
Purified Vi capsular polysaccharide of salmonella typhi 0.025mg, phenol 1.25mg |
NEWGEN |
0.5ml |
290.00 |
||
|
TYPHIVAX i |
Purified Vi capsular polysaccharide of |
AVENTIS |
0.5ml |
290.00 |
||
|
nj |
salmonella typhi 0.025mg, phenol 1.25mg |
PASTEUR |
||||
|
VACTYPH |
inj |
Purified Vi capsular polysaccharide of |
ZYDUS |
0.5ml |
200.00 |
|
|
salmonella typhi 0.025mg, phenol 1.25mg |
VACCICA |
|||||
|
RE |
||||||
|
VACTYPH |
inj |
*urified Vi capsular polysaccharide of |
ZYDUS |
5ml |
1800.0 |
|
|
salmonella typhi 0.025mg, phenol 1.25mg |
VACCICA |
0 |
||||
|
RE |
||||||
|
Contributed |
by: |
|||||
Dr. Shalini Chandan, Family Physician
Case Reports
Recurrent angioedema, urticaria with associated symptoms and signs of autoimmunity Ilhaam Ashraf, Balachandra *V, Ramakrishna Prasad, B. C. Rao
Abstract
A case of distressing recurrent angioedema of neck and oropharynx with involvement of skin and intestines in a steroid dependent uncontrolled diabetic who was treated s*ccessfully with omalizumab is presented.
Introduction
Angioedema shares common etiological background with chronic urticaria, both showing high levels of IgE. Associated conditions such as rhinitis, GI symptoms such as diarrhea and vomiting may also be present. Our patient presented with nodular skin lesions and a past history of wheals, the lesions were atypical of chronic urticaria. Biopsy of the skin lesion suggested urticarial vasculitis. The GI symptoms of acute episodes of diarrhea made worse by eating wheat preparations necissated investigating for possible coeliac disease which proved negative. A CT abdomen was n*t remarkable and endoscopic ideal biopsy showed lymphocytic infiltration. Though the diagnosis of angioe*ema was clear it was tough to correlate other symptoms with this diagnosis.
Case report
In June 2017, a 49-year-old man presented with frequent episodes of painful neck swelling and difficulty swallowing. The onset of these symptoms was --- in the past along with history of acute episodes of diarrhea and skin eruptions. These were presently under control with daily 8 mgs of Medrol. however, this had resulted in his diabetes going out of *ontrol.
Any attempt at reducing the dosage of Medrol would promptly result in an attack of acute angioedema.
His records showed the following investigations done in chronological order.
8/12/16 upper GI endoscopy mild gastritis. CLO test negative
10/12/16 US abdomen stratified thickening of wal*s of terminal ileum? infective ileitis.
14/12/16. Colonoscopy. Mildly inflamed mucosa in the terminal ileum. Ileal biopsy. Nonspecific lymphoid hyperplasia.
1*/12/16 CT Abdomen and pelvis Essentially normal
09/1/17 WBC 8700, FBS 110 mgs/dl
3/2/17 Acute rhinitis nasal pain and swelling of left side of the face of 4 days duration gradually becoming worse. CT brain and sinuses. Normal. Mild mucosal thickening in the right maxillary and ethmoidal sinuses 5/3/17 anti CCP Negative, RF positive 31 IU anti DS DNA positive
May17 episode of acute urticaria [photograph]
5/5/17 test for Anti Ds DNA n*gative, RA factor negative 8/5/17 Food intolerance test Allergy to cows milk
TSH levels normal, counts normal ESR 41
24/5/17 HIV, HBV, HCV Negative
Biopsy report from the papular lesion.
Perivascular and interstitial infiltrates of eosinophils and lymphocytes. Diagnosis: Urticaria Skin
6/6/17 Trans*horacic echo Normal
When seen on6/6/17 nodular rash front of the chest, acanthosis present, Systemic examination normal. Diabetes out of control [readings]
On 4mgs twice a day of Medrol
Ref to Dr B
Further tests. Spirometry normal, X ray chest normal. C-reactive protein 30mg/L. ESR35, Gluten allergen specific IGE negative
CI Esterase inhibitor functional> 90 normal
HTTG/DGP Screen 15.29 negative
Here is a patient, a mild well controlled diabetic, who was in good health till 8 months ago, when he developed acute episodes of diarrhea needing several admissions and extensive investigations. He subsequently had several episodes of acute urticaria and later a nodular rash present mostly on the front of the *hest. Around the same time, he began having recurrent episodes of angioedema involving face, n*ck and oropharynx. This necessitated the use of steroids and he had to take Medrol 4mgs twice a day to preve*t episodes of angioedema. This made his diabetes go out of control.
This was the situation when he sought help from us.
After extensive discussion involving the treating family physician, allergist and the patient, it was decided to offer him treatment with Omalizumab. He was given injections of this drug once a month subcutaneously for six months. His life-threatening episodes of angioedema disappeared even after the first injection and his dosage of methylprednisolone could be tapered off and stopped. His diabetes came under *ontrol.
At the time of reporting he is free of all the symptoms and his diabetes is under control
Discussion
Chronic urticaria and angioedema significantl* undermines the quality of life with indices of chronic urticaria patients closely resembling those of patients after a myocardial infarction. Patients have compromised day to day functioning in home management, personal care, recreation, social interaction, emotional factors, sleep, rest and work. Episodes of severe, life threatening angioedema can be a source of significant distress which need to be addressed as soon as possible. Furthermore, finding an effective therapeutic option in the face of multi system comorbidities like diabetes m*llitus can pose a clinical dilemma. Our patient had been havi*g urticaria with episodes of angioedema for the past 5 months and the prolonged steroid therapy to keep his symptoms from flaring up had affected his quality of life greatly. On the one hand, the steroids kept his attacks under chec*, but on the other hand, his glycemic control had worsened due to the same treatment. His case was a multidimensional puzzle of symptoms, systemic involvement, few therapeutic options and side effects. When patients present with a complex interplay of complaints like ours, the primary care specialist, often the first point of contact, has an important role to play in facilita*ing optimization of therapy thereby enabling diabetes control and a dramatic improvement in symptoms. In this context, the knowledge of therapeutic options like Omalizumab which has transfo*mative effect on patients with multi-system comorbidities is very important. Omalizumab, initially approved by the FDA for the treatment of patients with moderate to severe persistent asthma is now a well-established option in several treatment regimens for treating chronic idiopathic urticaria not responding to H1 antihis*amine therapy and angioedema. It is a monoclonal antibody that is directed against IgE. By binding to the Fc portion of the IgE molecule, it prevents IgE binding to its usual sites and blocks the entire sequence of ev*nts such as mast cell degranulation and histamine release that are implicated in IgE mediated hypersensitivity reactions. It is administered subcutaneously and clinical studies have shown that it causes dose d*pendent reduction in serum free IgE levels within 1 hour follow*ng the first *ose and maintained between doses.
Th*s case report seeks to address the importance of the knowledge of indications and usage of newer therapeutic options like Omalizu*a* as a drug that can give patients a c*ance at a better quality of life. However, it still has several unanswered questions. Were the episodes of acute diarrhea and the episodes of urticaria with angioedema separate entities or part of a common syndrome complex tri*gered by widespread activation of mast cells? Evidence suggests that patients wit* chronic urticaria may ha*e associated systemic manifestations in the form of fatigue, gastrointestinal symptoms, arthralgias etc. Omalizumab, by producing a rapid reduction in free IgE levels and subsequent decrease in high affinity IgE receptor (FcεRI) expression on mast *ells *nd basophils can alleviate these systemic symptoms as well. Although our patient’s gastrointestinal symptoms have not recurred since Omalizumab was given, there is ins*fficient proof to favour or disprove our hypothesis.
Secondly, the worsening of the bilateral pitting ankle oedema since the st*rt of Omalizumab therapy also remains unexplained. Whether it is an uncommon side effect of the drug itself or a result of the patient being well enough to return to his regular work hour which involves sitting for long periods, is still unclear. [this has since then greatly reduced.
References:
1168.x/epdf?r3_referer=wol&track*ng_action=preview_click&show_checkout=1&purchase_referrer=www.nc bi.nlm*nih.gov&purchase_site_license=LICENSE_DENIED
Correspondence: ilhaamashraf@gmail.com
Real time learning: POLYCYSTIC OVARIAN SYNDROME
Polycystic ovary syndrome (PCOS) is one o* the most common hormonal disorders among women of reproductive age, especially in those presenting with infertility. T*e exact prevalence of PCOS is not known as the syndrome is not defined precisely,but is highly va*iable ranging from 2.2% to 26% globally. There are very few studies conducted in India, but some done in South India and Maharashtra showed prevalence of PCOS (by Rotterdam's criteria) as 9.13% and 22.5% (10.7% by Androgen Excess Society criteria) respectively.PCOS was first reported by Stein and Leventhal in 1935, described as symptoms complex with amenorrhea, hirsutism, and enlarged ovaries with multiple cysts Polycystic means "many cysts," and PCOS often causes clusters of small, pearl-sized cysts in the ovaries. The cysts are fluid-filled and contain immature eggs. Women with PCOS produce slightly higher amounts of male hormon*s known as androgens, which contribute to some of the symptoms of the condition.
Early diagnosis of PCOS is important as it has been linked to an increased risk for developing se*eral medical conditions including insulin resistance, type 2 diabetes, high cholesterol, high blood pressure and heart disease. PCOS is an emerging health problem during adolescence; therefore promotion of healthy lifestyles and early interventions are required to prevent future morbidities.
Clinical features:
-
Infertility - PCOS is the most common cause of female infertility. Conception may take longer than in other women, or women with PCOS *ay have fewer children than they had planned. In addition, the rate of miscarriage is also higher in affected women. This being the most common presentation in women anxious to conceive.
-
Infrequ*nt, absent, and/or irregular menstrual periods- The menstrual irregularities in PCOS usually present after menarche being the most common presentation in adolescent age group.
-
Hirsutism -increased hair growth on the face, chest, back, thumbs, or toes – Scoring by Ferriman Gallwey score
-
Acne, oily skin, or dandruff
-
Weight gain or obe*ity, usually with extra weight around the waist
-
Male-pattern baldness or thinning hair
-
Skin tags(excess flaps of skin in the armpits or neck area)
-
Pelvic pain
-
Anxiety or depression
-
Acanthosis nigricans
Relevant history to be elicited in patients:
-
Menstrual history
-
Hirsutism/ Acne
-
Weight gain
-
Breast discharge/ headache
-
Social or emotional disturbance
-
Drug history- drugs which cause hirsutism ( like Danazol, Minoxidil, Cyclosporine, Progestin containing oral contraceptives, Diazoxide )
-
Family history- first degree female relative with PCO or males with premature alopecia or metabolic syndrome
Pathogenesis:
-
1. Chronic anovulatory state
-
2. Increased Luteinizing hormone ( LH) – due to increase pulse frequency and amplitude
-
3. Low normal Follicle Stimulating Hormone (FSH) – due to increased pulse frequency of Gonadotrophin releasing Hormone (GnRH) and negative feedback due to increased peripheral estrone.
-
4. Normal or modestly increased Inhibin B
-
5. Hyperandrogenemia due to premature adrenarche or impaired glucose tolerance and obesity
Relevant examination:
-
1. BMI
-
2. Secondary sexual ch*racters (Tanner staging)
-
3. Hirsutism
-
4. Acne (Grading by Indian acne association)
-
5. Acanthosis nigricans
-
6. Thyroid enlargement
-
7. Galactorrhea
Relevant investigations:
-
LH – elevated
-
FSH – reduced
-
LH/FSH > 3:1
-
Androgens – elevated
-
Sex hormone binding globulin (SHBG) – low
-
Prolactin – mildly elevated
-
Fasting Insulin levels – elevated
-
Glucose toler*nce test – abnormal
-
Lipid profile – dyslipidemia
-
TSH
-
Pelvic scan
-
Semen analysis and HSG to rule out other causes of infertility
Management by Family Medicine Specialist*
-
1. Diet, weight reduction
-
2. Exercise- 150 min/week
-
3. Evaluate for long term consequences
-
4. Sta*t Metformin
-
5. Contraceptives of choice:
When to refer to an obstetrician and gynecologist?
Refer when the patient seeks treatment for infertility, where further treatment like Ovulation induction with follicular scans, Clomiphene/ Letrozole and FSH/LH injections is needed.
Newer advances: Use of myoinositol.
-
Benefi*s of Myoinositol – improvement of insulin sensitivity and reduction of free testosterone, with an increase in pregnancy *ate.
-
Foods rich in Myoinositol – fruits, beans, corn, nuts.
Thanks to Dr. Swapna Bhaskar and Dr. Anita David for leading this case discussion.
Dr. Nidhi V. Nayak, Family Medicine Specialist email : nidhivnayak@gmail.com
Non Alcoholic Fatty Liver Disease [NAFD]
Case Report
A 38-year-old female presented to primary care clinic for routine health check with no symptoms.
Past history: No si*nificant past medical and surgical history
Drug history: None;
Family History: Not significant
Personal history: married, 2 children, Denies alcohol and tobacco use
Examination:
Wt: 80kg; height:160cm; BMI:31; BP- 110/70 mmHg, Pulse- 80bpm, afebrile, no anemia, jaundice, clubbing RS – Clear: CVS – S1 S2 heard. No murmurs P/A no tenderness, no hepatosplenomegaly.
Laboratory investigations:
FBS: 116mg/dl; P*BS:180mg/dl; HbA1C 6.9 *; Hb: 12.5gm/dl; WBC:4500; platelet count: 1,98,000; Total bilirubin: 0.5mg/dl, Direct bil: 0.3mg/dl; GGT:77U/L; ALP: 120 IU/L, protein: 6.4g/dl; Alb :4.2 g/dl; Creatinine:0.9mg/dl; Viral markers: negative ; HDLc : 28mg/dl; Total Cholesterol: 210mg/dl; LDLc: 144 mg/dl; Triglycerides:170
USG abdomen and pelvis: Mildly enlarged liver with fatty infiltration.
Serial monitoring of liver enzymes over a *eriod of 2 yrs. and various scoring systems for assessment of fibrosis.
|
DATE |
AST/ |
ALT/ |
APRI |
FIB4 |
NAFLD FS |
|
SGOT |
SGPT |
SCORE |
SCORE |
||
|
May 2016 |
115 |
138 |
1.3 |
1.92 |
0.7 |
|
July 2017 |
83 |
102 |
0.9 |
1.5 |
1.7 |
|
Oct 2017 |
118 |
143 |
1.3 |
1.89 |
1.75 |
|
Nov 2017 |
124 |
210 |
1.4 |
1.64 |
1.5 |
|
Dec 2017 |
184 |
242 |
2.0 |
2.27 |
1.69 |
Clinical problem
-
1) How would one can utilize these scoring systems in guiding NAFLD related decision making?
-
2) Which one is prefer most for *taging and monitoring?
-
3) Any specific thi*gs to keep in mind among south Asian populations?
Introduction
Nonalcoholic fatty liver disease (NAFLD) is probably the most co*mon liver disorder in the world, affecting 2.8-24% of the general population. It is a spectrum of disease from fatty liver to non-alcoholic steatohepatitis, fibrosis, and cirrhosis.t is also currently the most common cause of abnormal liver function tests and is recognized as a major ca*se of cryptogenic cirrhosis of liver. It is principally a disease of middle *ge and old age but at present, there is no general consensus *n whether *here is any predilection for a specific gender.
NAFLD is assuming higher importance now because of:
-
1. The possible role in the development of cardiovascular disease;
-
2. The association with diabete* and impaired glucose tolerance;
-
3. The strong relationship with metabolic syndrome.
NAFLD is closely related to obesity, type 2 diabetes mellitus and dyslipidemia, with a prevalence ranging from 50% to 90% in these patient groups[1]. The current dogma implicates that NAFL is a stable disease with or without a very slow* histologic progression over time, whereas NASH may advance to fibrosis and cirrhosis. However, several recent studies have challenged this view, demonstrating histological progression *lso in NAFL patients without histologic signs of NASH at baseline[2].
It is crucial for clinical management to obtain a prompt diagnosis of patients with advanced fibrosis because they carry an increased risk for developing complications such as hepatocellular carcinoma (HCC) or esophageal varices.
Diagnosis:
A diagnosis of NAFLD requires that there is evidence of hepatic steatosis on imaging or histology, and other causes of liver disease or steatosis have been excluded. Fibroscan (tissue elastography) is a new non-invasive modality in detecting liver fibrosis. But there are significant limitations to u*ing TE in NAFLD because of scarcity in availability, high cost and also results may be invalid in older patients (>52 years) and those with central *besity (BMI >35 kg/m2) or t*pe 2 diabetes.Its role in various liver diseases including NAFLD is still evolving. Till then, liver biopsy remains the only method for detection of fat and associated necro-inflammation and fibrosis (NASH) in the liver, and for grading and staging the disease in NAFLD. However, the majority of patients with NAFLD can be diagnosed and staged *dequately using non-invasive strategies. Liver biopsy should be used for subjects where there is diagnostic uncertainly or if non-invasive s*aging is indeterminate.[3]
NON-INVASIVE DIAGNO*IS OF ADVANCED FIBROSIS IN NAFLD Clinical and laboratory variables (serum biomarkers)
Clinical predictors of advanced fibrosis in NAFLD are male sex, Caucasian ethnicity, diabetes mellitus, obesity and increased aspartate transaminase (AST) or alanine aminotransferase (ALT) levels. However, there is a poor correlation between ALT levels and NASH, or the stage of fibrosis. In a study of 222 patients with NAFLD, 23* had normal ALT. The proportion of patients with advanced fibrosis was similar among those with normal an.d elevated ALT.AST is a better predictor for advanced fibrosis than ALT. In early studies on NAFLD, an AST/ALT ratio > 1 was found to be associated with advanced fibrosis.
APRI SCORE: AST: platel*t ratio index *APRI) with a negative predictive value of 94% to exclude advanced fibrosis (F3-4) in NAFLD. Another laboratory parameter related to fibrosis is serum ferritin. In a study of 628 patients with biopsy-proven NAFLD, elevated serum ferritin (> 1.5 × ULN) was associated with the diagnosis of NASH, high NAS, and development of advanced hepatic fibrosis.
NAFLD fibrosis score (NFS): For clinical de*is*on-making with the purpose of identifying patients with an indication for liver biopsy, several composite scores have been explored. In 2007, the NAFLD fibrosis score (NFS), based on six routine clinical parameters, was developed and validated in > 700 patients with biopsy- proven NAFLD[4]. The parameters are age, BMI, the presence of diabetes or impaired fasting glucose, the AST/ALT ratio, platelet count and albumin. A score below -1.455 has a high negative predictive value to exclude advanced fibrosis (stage 3-4), whereas a score > 0.676 predicts advanced fibrosis. Only patients in the indeterminate range between these two values need to undergo liver biopsy, thus avoiding up to 75% of biopsies[4]. In a meta-analysis from 2010, the pooled AUROC, sensitivity and specificity of NFS for the *etection of NASH with advanced fibrosis was 0.85 (0.80-0.93), 0.90 (0.82-0.99), and 0.97 (0.94-0.99). The NFS is endorsed by current American guidelines as a screening *est to exclude low-risk individuals from further *nvestigations.
BARD s*ore: It is based on three variables combined in a weighted sum (body mass index ≥ 28 represents 1 point, th* AST/ALT ratio ≥ 0.8 represents 2 points, and diabetes mellitus represents 1 point). A score of 2-4 had an odds ratio of 17 (confidence interval: 9.2-31.9) to determine advanced fibrosis and a negative predictive value of 96%.
The FIB-4 index: it was first developed for patients with hepatitis C and HIV but has been validated and compared with other non-invasive markers in a c*hort of 541 NAFLD patients. FIB-4 is based on patient age, AST, ALT, and platelet count. This index was superior to both NFS and B*RD in this specific cohort. An FIB-4 index ≥ 2.67 had an 80% positive predictive value, and a v*lue ≤ 1.30 had a 90% negative predictive value to diagnose advanced fibrosis.
Among the above-menti*ned fibrosis scoring systems the NAFLD fibrosis score (NFS) is the best-studied serum-based combined clinical algorithm; it was recommended in the latest American practice guidelines for NAFLD.
Are there any racial differences?
Because of ethnic differences in the occurrence of metabolic syndrome and its components, effect of ethnicity on clinico-pathological profile of NAFLD patients has been studied. One such study showed that the prevalence of insulin resistance, defined as the lower quartile of insulin sensitivity index, was approximately 2- to 3-fold higher in Asian-Indians than in other ethnic groups. Further, *sian-Indian men had an approximately 2-fold higher hepatic triglycerid* content and plasma IL-6 concentrations than Caucasian men. Majority of Indian patients with NAFLD are overweight or obese as per the Asian-Pacific criteria even though they do not have morbid obesity that is seen in Western patients [5]. Other differences in Indian patients include a lower frequency of metabolic syndrome including its components such as diabetes mellitus and hypertension, lower frequencies of iron abnormalities and HFE gene mutations, and presence of a histologically milder disease at presentation [5]. However, data on the natural history of NAFLD and the rates of seriou* significant chronic liver disease in such patients are lacking. Thus, there is a clear need for further prospective, cooperative studies. In conclus*on, NAFLD is responsible for significant liver disease in India. A lot has been done regarding the epidemiology, pathogenesis, diagnosis and treatment of patients with NAFLD. Yet more is required, to complete the various missing links.
References:
-
1. Ong JP, Younossi ZM. Epidemiology and natural history of NAFLD and NASH. Clin Liver Dis. 2007;11:1–16, vii.
-
*. Wong VW, Wong GL, Choi PC, Chan AW, Li MK, Chan HY, Chim AM, Yu J, Sung JJ, Chan HL. Disease progression of non-alcoholic fatty liver disease: a prospecti*e study with paired liver biopsies at 3
years. Gut. 2010;59:969–974. -
3. Anstee Q*, McPherson S, Day CP. How big a problem is non-alcoholic fatty liver
disea*e? BMJ2011;343:d3897.
4.Angulo P, Hui JM, Marchesini G, Bugianesi E, George J, Farrell GC, Enders F, Saksena S, Burt AD, Bida JP, et al. The NAFLD fibrosis score: a noninvasive system that identifies liver fibrosis in patients with
NAFLD. Hepatology. 2007;45:846–854.
5.Duseja A. Nonalcoholic fatt* liver disease in India—*s it different? Trop Gastroenterol. 2006;27:142–6.
Dr. Shalini Chandan, Family Physicia*, PCMH Restore Health & Sita Bhateja Hospital, Bangalore
drshalinichandan@gmail.com
My experience with Adult Croup!
A visit to a resort in Bangalore on 20 th May 2018, where my friends and I got into a swimming pool, gave me a lifetime experience of being a patient while being a doctor.
It all started with a th*oat irritation following the visit to the resort that lasted for 10 days and progressed to a laryngitis with pain and difficulty *n speaking, I did not have fever or running nose. On the 3 rd of June, I developed a cough with minimal expectoration. The cough progressed with increasing severity and expectoration. On the 7 th of June, while having a bought of cough, I suddenly had a stridor, where I could inhale, but could not exhale. And every inspiration was followed with a loud noise, typical of Croup. I rushed out of my room asking my family for help and they rushed me to a nearby hospital, where they took it to be just a case of acute exacerbation of asthma and started nebulization even without examining me. This increased my breathlessness and anxiety as I could not breathe. My family then decided to move me to a differ*nt hospital hoping for a better care.
At the ER of this hospital, I was given 200 mg of Hydrocortisone, Oxygen Inhalation with nebulization. Initial vitals were PR- 110 bpm, SpO2- 80 on room air, BP- 120/ 80 mm hg. CXR showed steeple s*gn, ECG- inverted T waves V2-4.

ENT resident came and performed indirect laryngoscopy and said there was moderate laryngeal edema. I kept telling ER doctor, that I am a physician, and I had a Croup with a feeling that something was stuck in my retrosternal area. But no one really seemed to be concerned about the croup. I was told by the ENT that I have a LRTI, and the attending Physician told me that my lungs were clear and I just had a laryngitis. They somewhere forgot me as a person and were diagnosing me *n parts! I was admitted for a day in the Hospital for observation and treated with IV Hydrocortisone 50mg TID (3 doses), Tab Augmentin 625 mg BD, and nebulization. Cardiac evalu*tion for inverted T wave was done but nothing significant but a feminine T wave inversion. I was discharged with advice to continue Tab Augmentin and multivitamin for 5 da*s. On my asking them about continuing oral steroids in view of Croup, * was told that since it’s *ust a laryngo-bronchitis and now my lungs were clear I did not require any oral steroids to continue. No one seem to be bothered about the diagnostic steeple sign in the chest radiograph!
After discharge, my symptoms persisted and in fact worsened. My sputum turned thick dark yellow and I developed fever of 101 ° F. The following day, I went back to ENT OPD as my symptoms were not improving and I could hardly speak. The consultant again did an indirect Laryngoscopy, and said my laryngeal edema was better than before, and advised to t*ke Tab Levoflox 500mg OD for 5 days along with Augmentin. My symptoms progressed and the next morning I again had a Croup after a bout of cough. That is when I wanted Dr. Ramakrishna Prasad to come and see me. He then said that adult Croup is uncommon but he had not seen a case so far. He then started on tab Prednisolone 40 mg OD which was slo*ly tapered. In the mean time I was also seen by Dr B C Rao, and he suggested Seroflo Rota haler 500mcg BD. While I am writing this, I am on 2.5mg Prednisolone to be continued for next 4 days and also Seroflo Rota caps to be continued.
My symptoms have reduced to 80%, with occasional cough, but still makes me breathless and still have to strain my voice to be heard.
What I Learnt:
-
1. Mental stress and anxiety faced by me and my family while trying to get emergency care.
-
2. [Being a doctor took immediate step to move to a better facility hospital. (then what about non-medical background people)]
-
3. ENT diagnosing it to be a LRTI and the Physician, bronchitis. When I am telling them that I have a Croup.
-
4. Specialist focusing only at a system and forgetting patient as a whole, where a Family Physician stepped in and saw me as a person with a holistic approach and played the bigger role and diagnosed it as Adult Croup (Laryngotracheitis). 1,2
-
5. Parainfluenza 1 is a most commonly identified organism in Croup in both children and adults. Had I taken my influenza vaccination, which I h*d been delaying, I would have avoided all this. So Adult vaccination is of utmost important for general population and more so for the doctors/ Physicians.
-
6. We as physi*ian should be willing to read literature on cases not commonly seen.
References:
-
1. A Narrowing Diagnosis: a Rare Cause of Adult Croup and Literature
Review. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5259656/ -
2. Uncommon presentation of a common disease: influenza A presenting as adult Croup. https://www.ncbi.nlm.nih.gov/pubmed/29866674
Dr. Ashoojit Kaur Ana*d, Clinical Director, PCMH Restore Health, Bangalore Email: ashoojit@gmail.com
Practice Experiences
The Story of Jennifer Lawrence
We family physicians have the privilege of g*tting visited by all sorts of varied profile people from different walks of life. One such incident I would like to pen down. I had a young robust lady in her early twenties who used to visit me for common ailments. Let me call her Jennifer Lawrence. She was an Anglo-Indian by origin. Th*re was one such day when she consulted me for fatigue. She was accompanied by her boyfriend/ live-in partner. On clinical evaluation, she had anemia. Deeper coaxing in history revealed she had taken some medications to get her missed menstrual periods from over the counter phar*acy. She had woken up in the ni*ht after noticing her bed wet, to soon realize she was in a pool of blood. She had taken abortion pills and had expelled the products of conception. Lucky for her she was not actively bleeding and reported to me with fatigue the next day. It was easy to treat her with basic investigations and oral medications and she recovered also. After this episode, she was continuing to be under my panel of patients for almost a decade.
She had become an entrepreneur and set up her own business of selling dental chairs and other medical chairs. I learnt from her that she was incurring heavy losses as she had to provide th* equipment first and the payments were made later. Mostly the chairs used to be returned without any sale for her.
After almost a year of having seen her last, one day she was accompanied by her aunt who is a nurse. She had developed a swelling in the left side of her neck. She was already evaluated by a physician *n the area, where she had moved into from the last one year. Having evidence for Tuberculosis from investigations, *he was put on anti-tuberculosis medications by her physician. She was visiting me this time to take help in countering the side effe*ts of the anti-tuberculosis drugs mainly fatigue. History revealed she was also noticing severe co*stipation from few months. I referred her to one of the tertiary hospital for Gastroenterology evaluation after which, she was diagnosed to be suffering from advanced stage rectal cancer.
She and her family members were not the only ones who were shocked with the finding. It included me and her other physician too. Her neck swelling which was being treated for tuberculosis had misled everybody in*o missing it as a secondary metastasis from the rectal carcinoma. There was no doubt that she had tuberculosis lymph nodes, but also a cancer of the rectum. The tertiary hospital helped her tide over her end of days and home managed her through the palliative department.
But in her last week of life, she visited me. Her emaciated look is *till in my memory. Her full decade of life I was associated with flashed in my mind. From th* day when she had bled in her bed to the present condition where she is aware of her death. She asked me how was I doing and introduced me to her uncle who was deep in grief. She left my clinic without any fear of death having accepted her fat*, teaching me some lessons to carry on in life.
Dr Syed Mubarak, Family medicine specialist. drsyedabu@gmail.com
Feature Article: Practice Mangement
How much should a doctor charge for a consultation? What is the value of 15 minutes of a doctor's time?
As an urban Family Physician in Gurgaon, I charge Rs 400 for a consultation, with free follow-up for 7 days after that. Home Visits are charged Rs 1000-2000 during day time (depending on distance), *nd Rs 1500-3500 at night.
Personally, I feel that I charge very less compared to the value I'm delivering to the *atients and their families. B*t I've realised, that from a business perspective, that feeling is largely irrelevant.
Wha* matters is
-
- *How much do I need to charge to cover my practice costs, and a decent standard of living for myself and my family.* From this perspective, there's no way I can survive just on consultation fee, I need to dispense medicines, go for Home visits, do mi*or procedures, collect lab sample and send to a lab, etc. All within the limits of ethics (no cutbacks from diagnostic centres or hospitals or pharma companies). Some doctors might be able to charge enough consultation fee to cover all that above. Other doctors might figure out other ways of augmenting their income, depending on their specialty.
-
- *How much value the patients get from the consultation.* This is the *ost interesting part. I've myself visited the "top" consultants of the city, paid Rs 1000-2000 for a single consultation, and came away dissatisfied, primarily because the doctor didn't deliver value proportionate to the consultation charge (not to mention the disproportionate wait time). A* doct*rs, we often restrict ourselves to our viewpoints, and keep cogitating on the ways we're excellent, and often forget to consider the patient's perspective. If the patient thinks they got more value than they pai* up, they're happy. If not, they're upset. That's the bottom line of any business, especially value-b*sed business like healthcare. The crisis in healthcare is not that doctors are charging too much, the crisis is that the patients feel that they are not getting services proportionate to what they've paid.
Let me illustrate that with an example. When I started my practice, people coming in for medical fitness certificates would often try to bargain. (Oh, it's just a 2-minute thing, why are you charging the full consultation?)
So we s*arted providing more value during the fitness check. For children and adolescents, a re-look at their va*cination records, vitamin D supplements for 10-16 year-olds, information regarding seasonal flu vaccine, height-weight plotted on a chart and shown to parents - which *nvariably leads to a discussion on diet and exercise, prescribe deworming, vision check etc etc. We've not had a single parent complain about the consultation charge since then. For others, a simple "anything else I can help with today" does won*ers!
There's lots more that can be done in each consultation! And the doctor doesn't have to spend too much effort e*ther - my Clinic Managers and my EMR do m*st of the things I mentioned above.
-
- *Patient's paying capacity* - India is a thousand Indias. And it's an interesting challenge how to deliver services to the poorest of the poor, and the richest of the rich. Each s*cio-economic stratum has its own paying capacity, and willingness to spend on healthcare services and p*oducts. I see families that consult me for their children, but go to the neighbourhood quack for their own health problems. I also see families who want me to spend the night at their home watching over their parent, and willin* to pay whatever I charge. As an entrepreneur, I know I can't grow if I ignore this reality, and as a doctor, it doesn't feel good to pick and choose patients based on their paying capacity. As a doctor-entrepreneur, my question is how I can deliver services that are affordable for the poor, and services that are top-notch quality for the super-rich, and something for everyone in between. Convenience and availability also figures in prominently in this equation.
Cross-subsidization often works, but only if there's a huge socio-economic gap between the people paying full fee, and those getting a subsidy. If there's only a marginal gap, then people start comparing and complaining.
Another solution I've seen work is to have a base consultation rate for everyone, and charge extra for premium services.
Don't forget "senior citizen discount" - they won't forgive you if you charge them the same as everyone else!
-
- *What is the competition charging?* There is no dearth of health services in India, regardless of what the NGOs etc would like us to believ*. We do not exist in isolation, and our patients are generally much more aware about the healthcare "market" than us. It helps to keep eyes and ears open to feedback from existing and new patients, and learn more and more about the "community of practice". Is everyone printing prescriptions using an EMR now? Then I need to be one step ahead and give my patients access to their record on my EMR! Has *veryone else increased their consultation fee? Then I need to hike mine too - as the patients' perception of qualit* often depends on how much the doctor charges!
-
- *The magic tou*h of the doctor.* We have a ve*y powerful tool with us - our behaviour! Giving patients full attention, taking a skilled history, performing a focused examination, explaining the differentials and prognosis in their language, and making the treatment plan in partnership with the patients and their families - all this not only improves patient outcomes, it also makes patients feel better. Furthermore, very often patients judge the quality of care they received based on the quality of communication of doctors and staff. "People may forget what you did for them, but they never forget how you made them feel!"
Bottomline, we can survive and flourish by providing a better *value proposition* to our patients than anyone else out there! Let's raise our standard of care and communication, understand our communities and competition better, and provide valuable services - then we would never need to feel defensive about what we charge!
Dr Devashish Saini, Founder and Family Physician, Ross Clinics & President Haryana AFPI devashish@ros*clinics.com
Masala
A distinguished colonel, who also presides over a state family medi*ine association, posted the picture below on International Yoga Day, 2018. Presumably, the intent was to engergize the ranks to be as fit as the leader himself was.

One can imagine the bewilderment when the treasurer of the association remarke* in alarm,
“Did not know you re*eive such a punishment at home sir!” "Well, what was the mistake?"

Technology-driven Primary Care – towards Universal Health Coverage For feedback please email viveksoukya@gmail.co*
It’s our immense pleasure to welcome you to Young physicians i* primary care update on the sidelines of 4 th national co*ference on family medicine and primary care on 2 nd -4 th of august 2019 (FMPC-2019) with the theme of “Technology innovation in bett*r delivery of Primary care in India” hosted by AFPI.
Target Audience: MBBS students interested in primary care, Physicians with postgraduate training, experience, or orientation toward* family medicine/primary care.
Healthcare sector has moved from traditional services to e-*ealth and now to m-health. Technology has now become a part of fabric of society so much so that, if we are not looking at technological solutions, we are not looking at solutions at all.
Just the way mobile devices could make major in-roads into remotest region of the country even when paved roads or piped water suppl* is not available. Similarly Technology driven primary care could be the solution to Universal Health Coverage. The ever increasing urban*rural divide in healthcare (80% doctors in urban region, 70% population in rural areas), poor doctor-popula*ion ratio (1:1800 against recommended 1:1000), high expectations of urban patients are the real problems. All of which can be tackled with transformative, transparent, equitable technological soluti*ns.
AFPI Karn*taka has been one of the most energetic *ltruistic organization, working for quality, ethical, and affordable primary care. The city of Bengaluru known for is metropolitan culture is the go to destination for most of the start-ups. The next leap in healthcare towards UHC is about to be hosted in Bengaluru by AFPI Karnatak*. The leaders of primary care in India are congregating in the silicone-valley to showcase, how futuristic innovations can transform the existing system to scale up to 21 st century standards.

This event with such a magnitude is planned to be organized with right amalgamation of various stake holders i.e. Government agencies, Corporate s*cial responsibilities, techies, healthcare start-ups, NGO's, public, paramedics, other medical specialties with the Young and dynamic Primary care Physician at the heart of it as a leader.
A 3 day event in month of Au*ust 2019 at the premises of esteemed Indian Institut* of Science (IISc) is sure to be for futuristic healthcare.
The entire event will be tailor made to reap maximum benefit with all the stakeholders. Carefully planned activities focused on active learning, with energizing and open discussion will be the standards to aspire. These learning are directed towards integration into day-to-day practice, in order to provide value addition.
Socially responsible Technologies
-
Person centered home care: using wearable devices
-
m-health, e-health
-
Bridging urban-rural gap
-
Telemedicine
-
Micro financing
-
Artificial Intelligence in healthcare
-
Electronic medical records and secure storage
-
Mobile apps in day-to-day practice
The meeting will also cover
-
Academic discussions
-
Improved patient management strategies
-
Me*tor-Mentee programme
-
How to set-up private practice
-
Facilities and experti*e to conduct primary care research
-
Viable career abroad
-
Pursuing subspecialty career paths- Diabetology, geriatrics, palliative care
-
Programmes offering further c*reer development- MRCGP, IGNOU, M.Med providing university
-
Career fest: Instant access to vacancies, job profile, pay package and working environment.
The goal of real healthcar* reform must be high-qualit*, universal coverage in a cost-effective way.
-
- Bernie Sanders
NOTE: This document has been prepared by a group of young family physicians as a part of the FMPC 201* planning process by AFPI Karnataka. The learning objective is to identify knowledge gaps in scaling up of primary care using the medium of technology. We urge the readers to participate actively in this process by corresponding your views and sug*estions to first author Dr. Vivek Karthikeyan (viveksoukya@gmail.com, +91-9986809582).
Welcome to AFPI Karnataka http://www.*fpikarnataka.in
THIS SPAC* IS OPEN FOR ADVERTISEMENTS