

AFPI KARNATAKA QUARTERLY NEWSLETTER
President’s Letter
Hello everyone.
I am very pleased to take this opportunity to wish our readership, members of the Editorial Team, all members of AFPI and their families a Very Happy New Year and would like to express gratitude to our readership for their support and contribution in 2018.
An honest reflection on the year gone by - Although early part of 2018 was quite eventful and promising, later part was a bit of disappointment. Though we have created a respectable place for ourselves through our high quality academic activities we have struggled to meet the expectations and accomplish resolutions made at the beginning of the year. However there’s something about the New Year that can be inspirational as the year will *oon be filled with activities, promises and a new opportunity to fulfill our commit*ents. We predict the year will be a busy one and challenging for AFPI Karnataka but I’m sure by working together, keeping focused on our priorities we can overcome the challenges and realize our ambitions. In my opinion 2019 is going to be the most *efining phase for our state chapter. We are hosting the 4th National Conference on Family medicine & primary Care (*MPC-2019). It is a matter of pride and honor for any state chapter to host a National Conference and we will not leave any stone unturned to make this a grand success. We wish to use this platform to showcase talent, bench strength and commitment of the state team to the cause of Family Medicine and primary care in India. It would be a great opportunity for the young FPs from the state to interact with renowned faculty and learn from the experiences of global leaders of Family Medicine.
As a prelude to the conference we would resolve to strengthen our academic collaborations, establish new partnerships, focus on evolving successful models of family practice driven by technology and innovations in li*e with the theme of the conference. It’s important for us to use our time wisely and move forward as decisively as we can till the conference and beyond in 2019. That will only be possible with your active participation, valuable inputs, continued support and teamwork. Once again my sincere thanks to the editorial of *his Newsletter for creating this platform of sharing knowledge and ideas.
Col (Dr.) Mohan Kubendra

Editorial Note
We bring *his issue out with much excitement. In October, 2018, Dr. Moh*n Kubendra, President of AFPI Karnataka, expressed his desire to see the AFPI Karnataka Newsletter become truly quarterly with issue* coming out on the first day of January, April, July, and October. We appreciated this suggestion
and are bringing out this present issue (Volume 3, Issue 1) on the 1 st of Jan, 2019.
We welcome with much pleasure, the addition of two new members to our editorial team, Dr. Akshay S Dinesh and Dr. Swathi S. Balachandra. Additionally, in keeping with the main theme, of FMPC 2019, we have introduced a new section on technology & innovations for better primary care.
Another highlight of this newsletter is that we have two research papers by Dr. Ilhaam Ashraf, a house
surgeon and Arjun Anand, 3 rd year medical student. Ilhaam’s article explores the issue of what
determines the career choice of medical students.
This newsletter also carries a practice experience where in a grave diagnosis was missed initially. Though it was not medical negligence, it resulted in the death of the patient, rupture of the doctor-*atient relationship, and significant anguish for the treating physician. While one sympathizes with the doctor’s anguish, such experiences are not uncommon and could happen to any doctor. We need to learn to deal with such scenarios instead of pushing these unpleasant experiences under the carpet. As always, the editors invite readers for their comments *nd send in their experiences.
2

AFPI-NEWS
National Conference on Family Medicine and Prim*r* care


3

Dr Roshni Jhan Ganguly nominated as the MRCGP INT South Asia Board member
AFPI Karnataka takes immense pride in sharing the news about nomination of Dr. Roshni as the South Asia Board Member on MRCGP INT. In addit*on to having o*tained the MRCGP INT herself, Dr. Roshni has served as an MRCGP INT exami*er, is part of the OSCE team for India. She has been an active contributor to AFPI since 20*3 and serves as one of the editors of this newsletter as well. We look forward to the impactful leadership she will bring in her new role. Congratulations Dr. Roshni!
K*runa Tru*t and AFPI Karnataka launch a new Primary Health Care Fellowship Program

Gleanings
Levosimendan
Congestive Heart failure is a common condition family physicians come *cross in their practice.
|
Levosimendan, |
is |
an intravenously |
|
|
administered |
treatment |
option for |
acute |
|
decompensated |
congestive |
cardiac failure |
and |
|
advanced |
heart |
failure. |
(1) |
It |
is |
a |
calcium |
|
sensitizer |
that |
also |
acts |
on |
adenosine |
||
triphosphate (ATP)-sensitive potassium channels. Levosimendan is an inotrope that acts without increasing oxygen demands and also causes coronary and systemic vasodilation.
In patients with decompensated congestive heart failure (CHF), IV levosimendan significantly reduced the incidence of worsening
4
CHF or death. This has been noted in double-blind, randomised trials. (2)
Common side effects of levosimendan include headache, hypotension, and nausea, secondary to vasodilation. It is useful to note that Levosimendan does not have significant drug-drug interactions with other medications used in the management of CHF including captopril, felodipine, β-blockers, digoxin, warfarin, isosorbide-5-mononitrate, and carvedilol.
Family phys*cians may consider using this drug or discussing this option when confronted with patients in decompensated congestive heart failure.

References:
-
1. Altenberger, J., Gustafsson, F., et al. Levosimendan in Acute and Advanced Heart Failure: An Appraisal of the Clinical Database and Evaluation of Its Therapeutic Applications. Journal of cardiovascular pharmacology, 2017 71(3), 129-136.
-
2. Pollesello P1, Parissis J et al, Levosimendan meta-analyses: Is there a pattern in the effect on mortality? Int J Cardiol. 2016 Apr 15;209:77-8
Technology and Innovation for Primary Care Practice
One of the qualities of a good primary care physician is that they use whatever tools are available to improve patient satisfaction and outcomes. Virtually every doctor (an* patient!) owns * smartphone and there are many applications tha* can be installed on these which are very useful for the physicians in their practice* We describe here a few apps that we have seen being put to innovative use in practice.
WhatsApp Business
Although there are more than 200 million active WhatsApp users in India, not many are aware of WhatsA*p Business. It is an official application developed by WhatsApp themselves for businesses to easily and quickly communicate with their customers. In addition to all the familiar features that WhatsApp provides, WhatsApp Business allows you to create a profile where one can display the times when they are open, add*ess, and website. It can be operated through a number that is different
5
from your personal phone number. Even a landline number can be used. There are also other useful features like quick replies which can be used to send pre-composed responses. The biggest benefit is that your clients can message you from the regular WhatsApp application without any difference.
India Drug Index
This is an application that has a comprehensive list of drugs that are sold in India which can be searched by their brand name. In practice we commonly come across *rand names that we have not heard of or don’t remember the composition of. Apart from generic name, the app also gives the market price of the drug. Once the database is downloaded to the phone, the application works without internet connection as well. Drugs are even classified by their pharmacological categories
which allows one to see all
available options in a particular
category. CIMS India is a

similar applicati*n which is available f*r iPhones as well.
Shots Immunizations
This is an application by
the American Academy of
Family Physicians and
Society of Teachers of
Family Medicine. It very
effectively displays the
various immunizations
that are needed at
different age groups and
in different profiles of
patients (including adult
vaccinations). There is an o*tion to view various recommended vaccines segregated according to conditions like HIV, pregnancy, CLD, etc.
MDCalc Medical Calculator

MDCalc is a collection of calculators that are useful in various specialities including in-patie*t management. These include al*orithms of management, calculators to diagnose or rule out diseases, and *rognosis. These calculators work offline as well. The app goes on to give next steps at the end of each calculation and also lists

out the references that were used to design the cal*ulator.
IAP Growth Chart
This app based on Indian Academy of Paediatrics data, allows tracking of growth of one’s pediatric patients. On entering the anthropometric details the app automatically generates the app*opriate graphs for length for age, height for age, weight for age, weight for length, and BMI for age. I* also gives an interpretation of how the child’s growth is progressing and gives a target to be achieved. The data can be saved and recalled during subsequent visits which makes it ideal for monitoring growth. Graphs generated can also be saved and shared with the parents.
While advancement in technology has genera*ed an e*ormous amount of relevant medical knowledge which is virtually impossible for any human to remember, the same technology has enabled a *hysician to accurately recall facts as and when needed through their internet connected smartphone. We should make the maximum use of these for delivering safe and timely care of global standards.
Dr. Akshay S. Dinesh,
Primary Care Physician & Programmer PCMH- Restore Health akshay@learnlearn.in
Family Medicine Education
Becoming someone’s Primary doctor
This is an e*perience with a patient that led to my learning as how to build doctor-patient relationship.
Mr. Mohith (name changed) was diagnosed with HIV, a *ew months ago elsewhere and was
started on tre*tment. He had come for a second opinion about his illness to us. I could see that he felt lost and had many doubts. He was sitting quite far from me, across the table with his relative being closer to me than him. I was finding it hard to ask him questions and I could
6
see that the same feelings were reciprocated in him as I got only superficial answers. In order to gain trust, I continued to have a detailed conversation and history taking, did examination in front of the relative, made the patient sit on a chair closer to me and then requested the relative to give me some time to talk to the patient alone. The relative agreed and sat out. That's when I could ask him about his real c*ncerns. That's when I felt real connection. And I think the same was reciprocated by him as he mentioned that he still couldn't accept the diagnosis, had doubts about it. No doctor had actually talked to him about it afte* diagnosis. His life had changed. My mentor had introduced himself and left me alone with the patient till this *oint, when he rejoined us. As I re*tated the patient's concerns to him and was trying to figure out how to address those, I was a bit confused. That is when my mentor suggested

to the patient that we would se* an agenda for the visit and told him genuinely that we will walk through this step by step and that we would be there for him. This reassured him. I told him that I wanted him to be okay with the diagnosis and that he will soon be healthy. He looked better. Then we did some tests and continued the consultat*on.
After he left, we did an exercise. My mentor wrote down important points that would help to build rapport, make a patient feel comfortable and respected, and the whole process of consultation more efficient. I had to rate myself 1-10 on those points. (listed in the box below) He rated me too. My colleague and our psychologist also shared the techniques they use out of their experience for each of these points and we had a valuable discussion.
Assessment parameters
-
1. Introduced herself
-
2. Ascertained the name of patient and person accompanying including relationship
-
3. Greeting in *ttempt to build rapport
-
4. Sought to conduct interview in private once some rapport was *stablished
-
5. Successfully sent the accompanying person out
-
6. Position of self and the patient to enhance communication
-
7. Body language
-
8. Set agenda for encounter
-
9. Open ended questions
-
10. Clarifying/elaborating questions
-
11. Comprehensiveness of the interview
-
12. As interview advanced, level of comfort the patient felt increased
-
13. Sought to determine what h* knows about his problem (his understanding)
-
14. Professional appearance
-
15. Documentation
-
16. Professional surroundings
7
As an intern in a government hospital, I had learnt to help the patients get through the system. To fill in the gaps. Like, teaching them how to take their prescribed medicines, how and where to get the investigations done. Talking to them about what their diagnosis was, and what was bei*g done and what they had to do was some*hing I did.
As a fellow in HIV at Vivekananda Memorial Hospital, Saragur, I learnt th*t care can be 100 X better with colleagues with the right attitude around. I learnt *ow to give holistic care. Since I was seeing OPD patients on not a regular schedule, i* was only rare to see the same patients in the opd in a planned manner. So every patient I saw, I'd make sure I gave them all the information, and advice they needed. I never was a primary doctor to anyone except a few of the* who valued my care and stuck to me over the phone. But it was never a plan. I never asked anyone to come back and see me next Monday or so. (Not that this experience was bad, but not enough for learning how to be someone's doctor)
But now, I have the time and space to build relationship with my patients. To ask them to follow up. To go slow and not bombard them with information.
Starting to think of every patient as my own and plan accordingly.
My colleague has built his practice bea*tifully. He told us how he remembers some important details about the lives of his patients. No* just their symptoms, but w*o they are, what they like, what they're going through etc. He used *o make notes before. Now it's become natural to him.
So, out of all the discussions, these are a few important learning points-

-
1. In order to build rapport, we often call the patients by their names. What happens if someone’s name is difficult? Ask - "What shall I call you as?" or be honest and say, "I'm having difficulty in pronouncing your name, what do you prefer? Help me with it" etc. It shows respect.
-
2. Keep a sheet to scribble important things you want to remember.
-
3. After sending out the relative, I had to explain to the patient why I did so. Something like "sometimes for some reasons, we can't be completely comfortable with mentioning everything to our relatives* So I sent him out. What you share now, will remain within this room."
-
4. Asking the pa*ient "how much time do you have". This will not only give them a sense that we value their time but also help us plan our agenda.
-
5. "What is your main concern?" always works.
-
6. I have this problem of doc*menting simulta*eously while talking. But a smart way would be after the intense sharing that the patient does, we can write with involvement of the patient. Something like "Ah, so these are
your main concerns (writing and showing the
patient), am I *ight?"
-
7. Always ask them to follow up
Dr Swathi S Balachandra
HIV & Primary Care physician, PCMH-Restore Health, Bangalore
Clinical Research Fellow, National Center for Biological Sciences (NCBS-TIFR)
email- swathisb01@gmail.com
8

Research Papers
Career Choices and the Indian Medical Graduate
Ilhaam Ashraf, House Surgeon, Bangalore Medical College & Research Institute, Ba*galore Correspondence: ilhaamashraf@gmail.com
What do you see yourself as 10 years from now? The questionnaire was focused towards students
A surgeon? An obstetrician? A doctor in the armed forces? A hospital administrator? A family physician? A public health specialist? An IAS officer? This qu*stion is often posed to students who are finishing their MBBS and preparing to step out of medical school, and into the seemingly uncertain future that awaits them. T*is is the time when a lot of them actively put in time and effort to brainstorm, soul search, and seek advice and guidance in the process of charting a favourable course through these otherwise murky, confusing waters.
Some questions like these were put forth in the form of an online questionnaire to a batch of medical students pursuing their internship in a government medical college in Bangalore, Karnataka. The questions were form*lated after a series of conversations with several medical students with the aim of discussing and identifying some of the possible influencing factors that help a medical student decide his future career path. Similar questions have been put forth to medical students in various phases of training acros* colleges in India and elsewhere through the years. However, all of those that the author could find focused singularly on the factors influencing a medical student’s choice of specialty and did not take into account the very real possibility of a medical student wanting to pursue something completely different and unrelated to the medical field following their graduation. With a young, dynamic and determined group of youth ready to step out in an ever evolving, open and fluid career space, acknowledging the existence of *his possibility is important, now more than ever before.
in their internship because it is a period following which the student usually has to make a very ‘real’ and concrete decision regarding his/her choice of career, and work towards implementing the decision whereas choices made by younger students often tend to change with time and experience as has been seen through previous studies. Interns had to answer the open ended question of ‘*here do you hope to see yourself in 10 years professionally” and then had to choose among a set of 15 options, those that they considered to be influencing factors in their decision. There was an open ended ‘Others’ option given as well. The respondents then *ad to prioritize their selected options in the order of priority.
Of the 25 respondents, 56% were male and 44% were females aged between 22-24. All the respondents were in their internship phase of MBBS in Bangalore Medical College and Research Institute, Bangalore, Karnataka. Among the respondents, 52% wished to pursue medical specialties includ*ng general medi*ine, cardiology and pediatrics while 32% expressed an inclination towards surgical fields such as general surgery, ObG and orthopaedics. There were respondents who wished to join the civil services, become hospital administrators and pursue further research. One respond*nt was undecided. More males than females preferred s*rgical fields while the results were almost equivocal when it came to choosing a medical special*y. Notably, all respondents who chose non-traditional career options such as civil services and hospital administration were male.
When it came to the factors influencing this choice, interest in the subject topped the list with 80% respondents selecting it as an option
9
and 60% of them assigning it the first in their order of priority. This was followed by

An interesting and new result that emerged from this study was the fact that several students

Reputation/Respect (60%), prospects of growth opportunities in the field (40%), flexible work hours and monetary gains (36% each), a call to service and respecting the wishes of t*e family (24% each), role models/influencers/mentors and domestic responsibilities (20% each). Future guidance and mentorship, research opportunities, travelling and exposure to, and awareness about the field were each options selected by 16% of respondents while entrepreneurship was selected by 14%. More females than males chose ‘domestic responsibilities’ and ‘respecting the wishes of the family’ as influencing factors.
From the above results, a few things become clear. A gender predominance towards choosing surgical specialties continues to exist, with males more likely to c*oose surgical specialties *han females. Although the gender gap has been *ecreasing, the trend remains consistent with findings of several studies done through the years. Furthermore, domestic and familial concerns continue to be viewed as a female dominant influencing factor which could influence professional roles and equity of responsibility in the family for these future doctors.
chose non-mainstream options such as hospital administration, pursuing research and joining the civil services which has not been taken into account in most studies done earlier. Entrepreneurs*ip opportunities were an influencing factor for 14% of respondents. This is of importance because it signifies a shift in conventional ideologies of career options that are limited to doing a conventional post graduation in a particular specialty as the only viable option after a medical degree. It was also heartening to see that there were respondents who showed an inclination for basic sciences and research which has always been chosen as a low priority according to several o*der studies conducted. However, all respondents who chose these above mentioned options were male which makes one concerned about the possible reasons that seem to be subtly yet surely stopping females from making more non*mainstream choices when it comes to a career which requires some looking into in depth.
Primary care and publ*c health had no takers in the study which remains an unfortunate reality in a country that is in definite need of a more robust primary healthcare system. The fact that
10
this trend does not seem to have changed through the years, with older studies reporting similar results, sp*aks o* a system that has failed to reinvent itself to attract the interests of the younger generation of doctors, and highlights a need to focus on ways to ensure that primary care b*comes a viable and meaningful option for future doctors in the making. Policy changes for strengthening the system, investing i* better infrastructure and opportunities for growth are some of the ways of ensuring primary healthcare is also viewed as a career option that accords ‘Respect’ and provides ‘growth opportunities’ equal to other specialties as these were two important influencing factors that emerged from this study.
‘Exposure *o and awareness about the field’ in medical school was an influencing factor for several respondents. Interest in the subject was the topmost influencing factor with 80% of respondents choosing that option. For the primary healthcare system as well as for sp*cialties in India such as family medicine, awareness and exposure which is poor among Indian medical students (as seen in an earlier study), this represents a window of o*portunity to find ways to reach students early on while they are in medical school and introduce them to these possibilities that exist which generates interest and not only allows them to make more informed choices but also aids in strengthening these important links in the chai* of quality healthcare for all.
This generation of doctors are going to be the future of the Indian healthcare system in the coming years and what they choose will have a significant impact on the direction and ways in which this system will grow, which in turn will influence the nature of healthcare, the geography of health care, and the cost of healthcare being delivered, and in turn its accessibility to the Indian population. It becomes important, therefore to truly try and

get to the bottom of what this generation wants from a career and what factors influence this decision so that interventions can be introduc*d to ensure that from all those aspects, primary health care and specialisations stand at par with each other. It becomes important for the healthcare system to provide avenues for exposure and awareness to the various options that exist during the in*tial period of medic*l training to allow this generation the right to make a truly informed choice.
This study was limited by a small sample size and low heterogeneity of sample. However, it brings to the fore valuable insights which have the potential to be studied and understood further in a larger study and among more diverse participants.
*eferences:
-
1. Kumar A, Mitra K, Nagarajan S, Poudel B. Factors influencing medical students’ choice of future specialization in medical sciences: A cross-sectional questionnaire survey from medical schools in china, malaysia and regions of south asian association for regional cooperation. North Am J Med Sci 2014;6:119-25.
-
2. Smitha Bhat, Landric D’souza, Jeffrey Fernandez. F*ctors Influencing the Career Choices of Medical Graduates. Journal of Clinical and Diagnostic Research. 2012 February, Vol-6(1): 61-64.
-
3. S.H. Subba, V.S. Binu, M.S. Kotian, N. Joseph, A.B. Mahamood, N. Dixit, A. George, P. Kumar, S. Acharya, P. Reddy Medical Education: Future specialization interests among medical students in southern India. The National Medical Journal Of India Vol. 25, No. 4, 2012.
-
4. Ilhaam Ashraf, Wendy W T Chan, Ramakrishna Prasad, Mohan Kubendra, D Hemavathy, Shailendra Prasad. Family Medicine: Perception and attitud*s among Indian Medical Students. Journal of Family M*dicine and Primary Care Vol. 7,No. 1, 205-209, 2018.
11

Peer Pressure in Adolescents – A Qualitative Study Exploring Perspectives of the Community about Peer Pressure in Adolescents.
Arjun Anand, 3rd year MBBS student, Basaveshwara Medical College, Chitradurga Correspondence: arjunanand500@gmail.com
Abstract
Background
Peer pressure holds strong influence on adolescents. However, the outlook on peer pressure v*ries from community to community. This study aims to understand the outlook on peer *ressure of students and parents of adolescents.
Materials and Methods
In this qualitative study, participants were asked to answer a scenario based semi structured questionnaire. Data were analyzed using framework analysis method.
Results
From the answers to the scenario, it was found that majority of the participants recognized that peer pressure played an active role in the lives of a*olescents which if negative and left unattended may lead them into drug or alcohol abuse, anti-social behavior and similar dangerous co*sequences.
Conclusion
The community understands that peer pressure plays an important role in development of adolesce*ts. The negatives of peer pressure must be curtailed with suitable steps to ensure the confiden*e and productivity of an adolescent mind is not lost. Counselling, parental supervision, guidance and positive reinforcement should be the norm when dealing with an affected adolescent.
Keywords
Peer pressure, adolescence, community outlook. Introduction
Adolescence is defined as a complex, multi- system transitional process involving progression from immaturity and social
dependency of childhood into adult life with the goal and expectation of fulfilled developmental potential, personal agency, and social
1
accountability . This transition exposes the
person to a multitude of issues such as peer pressure, emotional imb*lances, stress, substance abuse etc.
Most previous research has focused on processes related to peer pressure and its negative effects on adolescent development
2,3,4 .
H*wever, very little is known about the characteristics that make teens more prone to it 5 and the outlook of the community.
This study aims to explore the outlook of individuals on the influence of negative peer pressure and its effects on an adolescent in a challenged situation.
Methods
The study was done using an online survey of a scenario based questionnaire with open ended questions regarding the situation depicted in it. The participants were asked to answer the question* in their own words without a word limit to gain insight to their perspectives about peer pressure and its ef*ects on adolescents, as well as their viewpoint on the possible solutions to this problem.
Study sample
S*nce the study was aimed at understanding the opinion of the collective community, we encouraged people of all ages, sex and b*ckground to take part in the study.
The participants were recruited online via social networking sites and also by forwarding the questionnaire link to kith and kin.
Data collection
Prior to answering the scenario based questionnaire, participants were asked to fill out
12
a few personal details which included their age, gender, education level and current occupation.
They w*re then asked to proceed with the scenario and answer the questions that followed to gain insight into their views on the scenario given to them.
Data analysis
The answers were categorized based on their relevance and repetitive occurrence and were tallied to the number of responses given till no new concepts were obtained. The answers to the *ive questions were tabulated and illustrated in the form of charts for easier analysis and understanding.
Results
A total of 146 responses were received from participants of various ages and background in order to incorporate various outlooks to the scenario.
Out of the 146 participants, 32.7% were males and 67.3% were females. Of the 146 participants, 37.2% were adolescents and 62.8% were adults. All participants were literate. 28% were graduates, 53% were postgraduates, 9.8% were in Pre University and 9.2% were attending school.
Interpretation of the results
A scenario was given to the participants to assess and answer the open ended questions that followed. The scenario consisted of a regular, studious adolescent falling prey to bad company leading to academic and personal misconduct.
The charts given below illustrate the responses given by the participants to the questions asked.

Chart 1 gives the responses when asked to
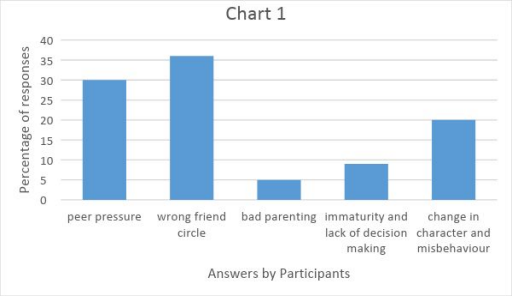
“identify the central problem highlighted in the scenario”.
Majority of the participants identified two central themes- 36% quoted that the problem arose due to wrong friends’ circle and 30* estimated that the problem was peer pressure. 20% were of the opinion that the problem was change in character and misbehavior, 9% identified it as immaturity and lack of decision making skills of the adolescent, while 5% suggested it was bad parenting.
Chart 2 illustrates the responses given when
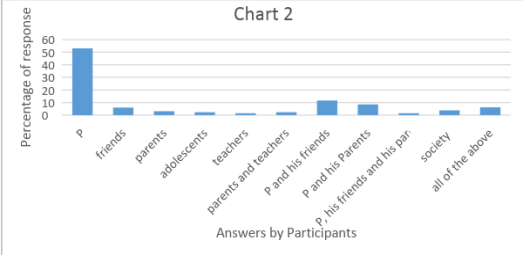
asked to “identify the *roblem causer *n the scenario”
More than half the respondents (53%) declared that the adolescent in the scenario was the sole culprit.
11% stated that it was the adolescent and his friends’ circle, 8.5% claimed it was the adolescent and his parents, 6% said it was the fault of only his friends, 3.18% urged that it was the society, 3.1% attributed it to so*ely the parents, 2.3% blamed the adolescent phase of life and another
13
2.3% said the parents along with the teachers should share the blame. 1.5% said it was the fault of the adolescent, his teacher, his friends as well as his parents, while 6.2% decided to include all the above reasons in their statement.
Chart 3 illustrates the responses given when asked to “identify the cause for the problem in the scenario”
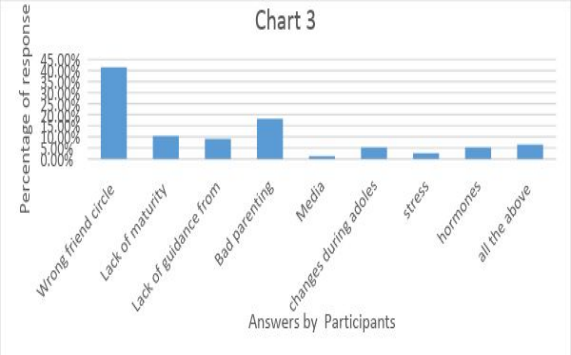
About 41% held the friends’ circle responsible while 18% blamed it on bad parenting. And 10% declared that it was the lack of maturity that was *o be accounted, 9% stating it was the lack of guidance from teachers and parents, 5% claimed it was due to the hormonal imbalances and adolescent changes. 2.6% and 1.3% of the pa*ticipants claimed it was due to stress and media respectively. About 6.5% of them responded that i* was multifactorial and all the above causes should be taken into consideration.
14

Chart 4 illustrates the responses given when asked to “state the consequences for the
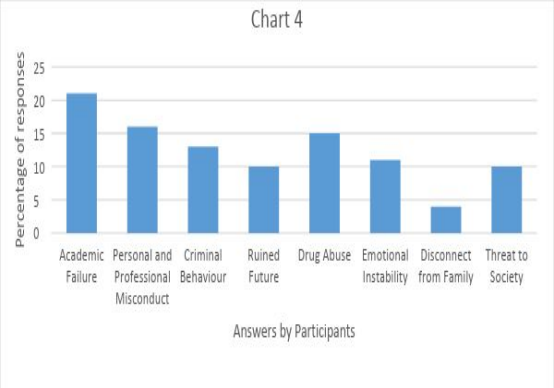
problem in the scenario”
When asked about the consequences, 21% said it would lead to academic failure and likely drop
out, 16% stated that it would cause perso*al and professional misconduct, 15% deduced that the adolescent would give into drug abuse and addiction. About 13% clai*ed that the adolescent would exhibit criminal behavior in the future while 11% reported that it increases risk of emotional instability. 10% predicted a hazardous future for the adolescent and another 10% expected him to be a threat to society while 4% claimed he would be disconnected from the family.
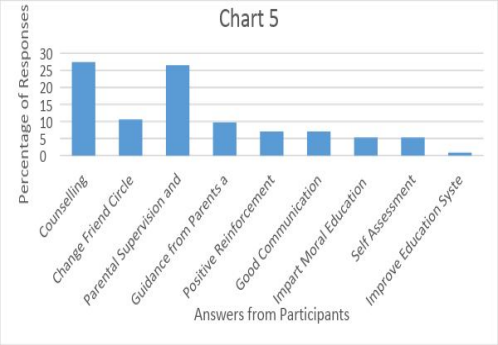
Chart 5 illustrates the responses given when asked to “suggest solutions for the problem in the scenario*
Most of the participants advised counselling (27%) and parental supervision and support as the best solution. Other solutions include change of friend circle (10%), guidance from parents and teachers (9.7%), positive reinforcement (7%), good communication from teachers and parents (7%) imparting of moral education (5.3%), self-assessment (5%) and improve the existing e*ucation system (0.8%).
Discussion
Adolescence is a pha*e distinguished from both childhood and adulthood. UNICEF has deemed adolescence as a transitional period that requires special attention and protection. Physically and mentally, adolescents go through a number of transitions while they mature. Social influence is the effect others have on an individ*al or a
group with respect to their attitude* and behaviour 6 . There are different mechanisms of
mutual influence process, and one of the most frequently referred to mecha*isms is youth peer pressure. Peer pressure is often used to transmit group norms and foster loyalty to the
7
group . However, there is the negative aspect of peer pressure that leads adolescents into harmful vices. Because they want to be
acknowledged by their peers, teenagers may willin*ly disregard many of the norms, values, attitudes, and behaviours learned *reviously
8
from their parents, siblings and teachers .
*mpirical *esearch has shown an increase in risk factors, such as peer pressure 9 , for substance abuse by adolescents. Hence it’s an emerging problem that the community needs to be aware of.
The result shows tha* majority are aware of the negative peer influence teenagers face. They recognize the delicate nature of the adolescent mind which is susceptible to the negative influences that they might face and also the willingness to disregard the lessons learnt by them from parents and teachers in order to gain acceptance from thei* peer group. They not only blame the child alone but also acknowledge

that parents and teachers play an important role to prevent this.
Some studies show with indirect relevance that
|
10 inclin*tion for violence , aggression levels |
1,12 , |
|
and |
delinquency |
13 |
increase |
with |
age |
in |
adolescents. Hence the right approach would be to identify and assess the situation at the earliest to avoid them maturing into antisocial adults.
Our study found that counselling as well as positive reinforcement with supervision from the parents and teachers was one of the most
commonly suggested solutions by the community members. Other studies have
shown that the adolescents who participate in social activities were found to have lower peer
14
pressure levels . Participation on the part of adolescents in sports, social* and artistic
activities at school does not only increase the positive notions of school life, but it also makes it easier to rectify behavioural i*sues 15 . It is of paramou*t importance to change a student’s negative social and cultural environment 16 and provide all of them with the facilities and opportunities to participate in non-curricular activities at school. Thus, the students are given a segue to add positivity to their life, which could help reduce negative peer pressure behaviours. It would also be *seful for school management and counsellors to conduct various events encouraging students to perform sports, cultural, social and artistic *ctivities 17 and to cooperate with social instit*tions for this purpose.
Conclusion
The aim of the present study was to analyze the perspectives of the community to peer pressure faced by adolescents and to explore their solutions.
The most important conclusion to be drawn from this study was that they recognized peer pressure as a cardinal issue that may lead adolescents to misbehave and they have been able to identify the causative factors without completely blaming *he adolescent. They have also stated reasonable solutions to this obstacle, of which counselling and parental intervention are foremost. Adolescents have a developing and delicate mind that needs to be dealt with
15
patience and care which have been strongly emphasized by the community.
Declaration
No conflicts of interest References
-
[1] Greenfield, P. M., Keller, H., Fuligni, A., & Maynard, A. (2003). Cultural pathways through universal development. Annual Review of Psychology, 54, 461-490.
-
[2] Berndt, T.J. (1979). Developmen*al changes in conformity to peers and parents. Developmental Psychology, 25, 458-464.
-
[3] Brown, B.B. (1999). Measuring the peer environment of American adolescents. In S.L. Friedman & T.D. Wachs (Eds.), Measuring environment across the life span: Emerging methods and concepts (pp. 59-90). Washington, DC: American Psychology Association.
-
[4] *antor, D.A., Messervey, D. & Kusumakar, V. (2000). Measuring peer pressure, popularity, and co*formity in adolescent boys and girls: Predicting school performance, sexual attitudes, and substance abuse. Journal of Youth and Adolescen*e, 29 (2), 163-182.
-
[5] Allen, J.P., Porter, M.R. & McFarland, F.C. (2006). Leaders and followers in adolescent close friendships: Susceptibility to peer influence as a pr*di*tor of risky behaviour, *rie*dship instability, and depression. Development and Psychopathology, 18, 155-172.
-
[6] Berkman LF. Social support, social networks, social cohesion and health. Social Work in Health Care. 2000;31:3–14.
-
[7] Vander Zanden, J.W. (2000). Human Development. New York: The McGraw-Hill Companies.
Case Reports

-
[8] Lebedina Manzoni, Marija & Lotar Rihtaric, Martina & Ricijas, Neven. (2011). PEER PRESSURE IN ADOLESCENCE - Boundaries and Possibilities.
-
[9] Allen, *. P. Chango, J., Szwedo, D., Schad, M., & Marston, E. (2012). Predictors of susceptibility to peer influence regarding substance use in adolescence. Child *evelopment, 83(1), 337- 350.
[10 ]Balkıs, M.; Duru, E. & Buluş, M. (2005). The relationship between attitudes toward violence and self*efficacy, media, *eliefs toward violence, peer group and sense of belonging to school. Ege *ğitim Dergisi,6 (2), 81-97.
-
[11] Hotaman, D. & Yüksel-Şahin, F. (2009). The analysis of elementary school students’ level of aggression according to school’ elements and some variables. E-Journal Of New World Sciences Acade*y, 4 (3), 833-858.
-
[12] Şahan, M. (2007). Predicting aggression levels in h*gh school students (Unpublished master’s thesis). Gazi University, Turkey.
-
[13] Fulya Yüksel-Şahin / Procedia - Social and Behavioral Scie*ces 191 ( 2015 * 1807 – 1812 1811)
-
[14] Yüksel-Şahin, F. (2013). Predicting delinquency levels in Turkish adolescents. Procedia Social and Behavioural Sciences, 89,841-847.
-
[15] Aydın, A. (2008). Sınıf yönetimi (Classroom management). Ankara: Pegem Akademi.
-
[16] Kızmaz, Z. (2006). A theoretical approach to the roots of violence behaviors at schools. C.Ü. Sosyal Bilimler Dergisi, 30 (1), 47-70.
-
[17] G*ve*, M. (2002). Roles and duties of counsellors in school safety. Eğitim Araştırmaları Dergisi, 9, 68-72.
Typhoid Hepatitis-A Diagnostic Dilemma
Abstract: An unusual case of Typhoid hepatitis which posed diagnostic challenges in the treatment of Typhoid fever managed successfully in Primary care clinic.
Introduction
Typhoid fever is a very common infectious disease of tropics, associated with high morbidity and mortality. It usually starts as an
16
acute disease without localization, and is clinically indistinguishable from other infections, including malaria, bacterial, and viral infections. Multiple *rgans are known to be affected by the disease. Typhoid fever is often associated with hepatomegaly and mildly deran*ed liver functions but a clinical picture of acute hepatitis is a rare presentation. Hepatic involvement could be considered important, as it may be associated with a higher relapse rate. We report a young patient who presented with fever and jaundice and was found to have acute hepati*is secondary to typhoid fever.
Case Report
A 36-year-old male patient was referred by a fellow practitio*er with history of high-grade fever with chills of 5 days duration on 30 th June 2018. There was no history of cough, chest pain, dyspnea, dysuria, diarrhea, skin rashes, pruritus, dark color urine, clay color stool, or *ny hemorrhagic manifestations. He had no significant history of medical illness, drug ingestion, surgical procedures, blood transfusion, sexual promiscuity, intravenous drug abuse. He gave a hist*ry of alcohol consumption in moderation. On examination, he was ill looking, mildly dehydrated, and febrile. He had tachycardia with normal blood pre*sure and respiration. Rest of the general and systemic examination was unremar*able. His laboratory investigations done by the previous doctor showed b*rderline leukopenia
3
(3860/mm ) and thrombocytopenia (90,000/
3
mm ) Peripheral smear for malarial parasite was negative.
A detailed history of the present illness revealed that he had high grade remittent fever with chills and temperature ranging from 103℉ to 104℉ with a typical stepwise patt*rn, characterized by a r*sing temperature over the course of each day that drops by the subsequent morning.
The blood *ultures and serology for enteric fever and dengue were sent.
IgM for Typhoid was positive in 1:320 dilution for “H” antigens. The serology for dengue sent earlier was negative. Patient was empirically treated with oral Cefixime 200mg twice daily

and Azithromycin 1g oral daily awaiting blood culture repo*ts.
His blood culture yielded a growth of Salmonella typhi after 3 days incubation, with antibiotic sensitivity to Azithrom*cin (17mm), Ceftriaxone (25mm), Ampicillin(25mm), and Chloramphenicol (23mm). The strain was resistant to Ciprofloxacin.
Biochemical evaluation showed normal renal function and electrolytes, albumin, and coagulation parameters.
Transaminases were elevated with aspartate aminotransferase (AST) 381 U/l, alanine aminotransferase (ALT) 304 U/l, Gamma G.T 235 U/L and alkaline phosphatase (ALP) 256 U/l. Total and conjugated serum bilirubin were 1.85 and 0.85 mg/dl, respectively.
The patient continued to be febrile after 3 days of antibiotic therapy and his liver enzymes showed worsening trend (AST level was 1112 U/l and ALT level was 848 U/l). The icterus was apparent c*inically, with a total bilirubin level of 6.32 mg/dl. Serology for viral hepatitis was sent.
Ultrasound abdomen revealed mild splenomegaly, borderline nonspecific lymphadenitis and terminal ileitis without any free fluid i* abdomen. Hepatic viral markers were negative.
Peripheral smear showed a picture of Normocytic normochromic anaemia with relative lymphocytosis.
With continued antibiotic and supportive therapy, the patient showed clinical improvement along with decline in liver transaminases levels. The patient became afebrile after 4 days, jaundice started improving, total bilirubin came down to 2.4mg/dl on the 7th day of therapy. Platelets increased to 92,000/cumm. There was no relapse of fever *ill 6 weeks from completion of therapy.
Discussion
Typhoid fever continues to be a common infection in the developing countries. William Osler initially reported hepatic in*olvement of typhoid fever in 1899.[1] Hepatomegaly and
17
moderate elevation of transaminase levels are the common findings that occur in 21–60% of cases[3,4] of typhoid fever. However, severe hepatic derangement simulating acute viral hepatitis is very rare. The presentation with marked elevation of transaminases similar to that of acute viral hepatitis, as observed in this case, has been reported by others.[2,6,7] Recognition of this clinical condition is particularly important in tropical countries where malaria and viral hepatitis are quite common. El-Newihi et al.[6] did a retrospective analysis to compare clinical, biochemical picture, and the outcome of patients with Salmonella hepatitis and acute viral hepatitis. They concluded th*t the clinical picture of Salmonella hepatitis is f*equently indistinguishable from that of viral hepatitis. Oth*r clues that raise the possibility of Salmonella hepatitis include high fever, relative bradycardia, and left shift of WBCs. Salmonella hepatitis responds to proper antibiotic therapy and has an excellent p*ognosis.
In viral hepatitis, nonspecific prodromal illness precedes jaundice and the fever usually subsides with the appearance of jaundice, while in typhoid hepatitis, jaundice usual*y occurs within the first 2 weeks of febrile illness and the fever persists despite the appearance of jaundice.[7]
Pramoolsinsap et al.[8] in their comprehensive review of Salmonella hepatitis suggested that typho*d fever is often associated with abnormal li*er biochemical tests, but severe hepatic involvement with clinical features of acute hepatitis is a rare complication. The documented incid*nce varies widely from less than 1% to 12% patients with enteric fever. The clinical course can be severe with a mortality rate as high as 20%, particularly with delayed treatment or in patients with other complic*tions of Salmonella infection. The factors predisposing to vary*ng degrees of hepatic injury in typhoid fever are not exactly known. Possibly, there is an interplay of the micro-orga*ism factors and the immunity, which cause liver injury.[9] The patho physiological mechanism by which Salmonella produces hepatic dysfunction, al*hough not fully known as yet, is *ostulated to be either due to direct invasion or by endotoxemia with

immune-mediated liver damage.[4] Histopathologic study of the liver reveals typhoid nodules, cloudy swelling, ballooning degeneration, moderate fatty change, and mononuclear cell infiltrate in few focal areas.[3] In addition, intact bacilli have been demonstrated in the parenchyma of the liver by immunohistochemistry and have been cultured from liver biopsy.[2]
In a study of 254 patients with typhoi* fever, Ahmad et al. [11] found that clinical manifestations of typhoid fever are often non-specific and clinically indistinguishable from other infections, including malaria and other bacterial and viral infections, and can pose a significant diagnostic problem, especially in the tropics where jaundice in the febrile patient can be due to malari*, amoebic or viral hepatitis. In many parts of the world, diagnosis is still based entirely on c*inical features because conclusive laboratory confirmation of the infection is not usually available. They also reported significant rise in serum bilirubin without a corresponding increase in serum ALT, which is unusual in viral hepatitis but common in typhoid. So, typhoi* should be considered in any febrile patient who develops jaundice ab*ut a week after the onset of illness and at *he peak of fever with or without hepatomegaly. There are studies showing higher relapse rate associated with Salmonella hepatitis as compared to the general pop*lation.[12]
Conclusion: Since typhoid fev*r is a common illness, the recognition of Salmonella hepatitis i* of clinical importance as it can m*mic viral, malarial, or amoebic hepatitis and pose diagnostic challenge. Early institution of specific therapy can improve the prognosis in these patients as it is associated with higher relapse rate.
Col (Dr) Mohan Kubendra,
MBBS, DNB(Fam Med), MNAMS, PDDM, DHHM
Spandana Healthcare
email: mohankubendra@gmail.com
18
References
-
1. Osler W. Hepatic complication of typhoid fever. Johns Hopkins Hosp Rep. 1899;8:373–87.
-
7. Nazm*l-Ahsan HA, Jalil-Chowdhury MA, Azharr MA, Rafiqeuddin AK. Pitfalls in the diagnosis of

jaundiced patient in the tropics. Trop Doc. 1995;25:191.
-
12. Khosla SN. Typhoid hepatitis. Postgrad Med J 1990; 66:923-
A Case of Multiple Infections
Introduction
We describe the case of a patient who had an acute f*brile illness with jaundice, leukocytopenia and thrombocytopenia, and whose laboratory investigations confirmed three different illnesses.
Case report
Our patient is a 30 year old priest who resides in a temple with potential exposure to contaminated water. He is a diabetic on oral metformin. He presented with fever, headache, nausea & vomiting, joint pain, dysuria, and high coloured urine and itching all o* which developed over the next three days. On examination he was febrile, had mild icterus, a coated tongue and his liver was palpable and tender.
Differential diagnosis of infectious hepatitis, leptospirosis, and dengue was considered and
investigations were ordered. He was found to have elev*ted l*ver enzymes (350s), elevated bilirubin (2.0mg/dl), leucocytopenia
|
3 (2600/mm |
), |
thrombocytopenia |
|
3 (1,09,000/mm |
). |
This |
was |
in |
addition |
to |
an |
ESR |
of 12mm/hr, Hb of 14 g%, with deep yellow coloured urine wh*ch also showed traces of albumin, bile salt and pigments. His Dengue NS1 was positive, Hepatitis A IgM *as positive and Leptospira IgM was also positive.
He was prescribed Doxycycline 100mg BD, Vitamin K, Ursodeoxycholic acid 300mg BD, Pantoprazole+Domperidone and Livina Capsules (an Ayurvedic preparation) on OPD basis.
He returned after two days with reduced fever, but increased icterus and lab reports showed *orsening liver function as well as platelet drop
3
to 75,000/mm .
The patient was then admitted to a hospital and treated with IV fluids, Inj. Glutathione BD, Inj.
19
Erythromycin, oral Cefuroxime 500mg BD, Methylprednisolone and Cholestyramine sachets.
His platelets returned to normal by 5th day, bilirubin which had gone upt* 15.6 mg/dl and liver enzymes started decreasing by 8th day and returned to normal at the end of 2nd week. He was full* normal by 3rd week.
Discussion
Applyi*g the Occam's razor to clinical problems often pushes the clinician to look for one unifying diagnosis that explains all of a patient's condition. But, there are situations that demand cognizance of Hickam's dic*um that "A man can have as many diseases as he damn well pleases".
There are many algorithms of management o* acute undifferentiated febrile illness. In tropical regions, Dengue is ruled out early in diagnostic algorithms.
Various conditions can mimic the critical phase of dengue. These include acute abdomen, acidotic condit*ons, infections like leptospirosis and malaria, autoimmune diseases and malignancies. Leptospirosis and hepatitis have both been reported as concurrent infections with and causing atypical presentations of dengue.
In contrast with the management of dengue, leptospirosis is managed with antibiotics and therefore differentiating between them is important. While fever, myalgia, and headache are commonly seen in both illnesses, jaundice, hyperbilirubinemia, leukocytosis, and anemia are more common in leptospirosis. Similarly, rashes, positive tourniquet test, and thrombocytopenia are more likely seen in dengue.
Dengue often presents with liver involvement and even acute liver injury. But coinfection with viral hepatitis has also been reported. Serum aminotransferases are often elevated 8-10 times normal in viral hepatitis in contrast to 2-3 times their normal value in dengue.
Reports of hepatitis A and leptospirosis co infection also exist. Hepatitis A infection could

even predispose leptospirosis infection to p*ogress to Weil's syndrome. Like in dengue, transaminases are usually only in the hundreds in leptospirosis.
NS1 antigen alone or in combination with IgM has good sensitivity and specificity for the diagnosis of dengue. Dengue IgG is useful in differentiating between primary and secondary infection. A positive IgM test or high microscopic agglutination test (MAT) titre makes presumpt*ve diagnosis of leptospirosis. Confirmation of leptospirosis requires either four-fold rise in MAT titre, sero*onversion, being positive by any two different types of rapi* test, or isolation of spiro*hetes. Laboratory diagnosis of Hepatitis A is also through IgM which can remain positive upto 3 months (and rarely 6-12 months).
A cursory search of literature does not show any reported case of a coinfection of dengue, leptospirosis, and hepatitis A in a patient.
Conclusion
Acute febrile illnesses can be concurrent infections due to similarities in epidemiology. It is important to look out for a concurrent infection even with a confirmed diagnosis because of the complications they can lead to and also especially when there are worsening or unexplained symptoms or laboratory reports.
Dr. Srinath Herur
Family Physician,
email: herurs@gmail.com Inputs by Dr. Akshay S. Dinesh
References
20
Practice Experienc*s

Final diagnosis
We, doctors are often faced with the problem of diagnosing the patient’s illness. More often than not it is based on history and clinical examination alone and one can *et away with it. On some occasions one needs the help of lab tests, antibiograms, histopathol*gy on biopsied tissue to arrive at a diagnosis. In almost all cases this will help the treating doctor to arrive at the final diagnosis and initiate the required treatment.
But in rare cases even after all this, one can fail and face the consequent personal anguish and incur patients’ and relatives’ displeasure for *aving missed the final diagnosis.
Here is an experience that took place not so long ago in my practice.
I saw a 56 years old gentleman with the h*story of progressive loss of appetite of three months duration, loss of weight, low-grade fever, pain abdome*, indigestion with episodes of loose stools and constipation.
On examination, I found him looking exhausted, pale and depressed. Cardiovascular, respiratory, Nervous systems were normal. No lymph nod*s were felt. H*wever, on palpation, there was mild te*derness all-over the abdomen
He had undergone the following investigations
ESR; 42 mm/hr. HIV negative.
U/S scan abdomen: Chain of enlarged lymph nodes along the paravertebral region, in bilateral iliac fossae, measuring 10 to 15 mm.
Impression: Koch’s/malignancy.
He was advis*d CT guided biopsy and histopathology from one of the prominent lymph nodes. This was duly done and the report came as, TB lymphadenitis.
With all this information diagnosis of TB lymphadenitis was made and it was decided to start ATT-CAT-1.
Counselling done regarding TB, effects and side effects of ATT, the good prognosis and he was advised *o return for review after 15 days.
He and his relatives asked me whether to postpone the marriage of his daughter which was scheduled to take place in three months’ time. I confidently told them to keep the scheduled date a* the response to treatment is almost always excellen*.
Two weeks later he came with minor complaints of nausea, weakness, and did not show much improvement. Thinking about the possible liver injury, an LFT was ordered which came back as normal. The patient was reassured and told that
21
it will take some more time for him to get better.
This went on for two months with no improvement. Investigations repeated including an abdominal ultrasound scan. All the reports were within normal limits but the scan showed, compared to previous scan some nodes are enlarged and some showed central necrosis.
Keeping in mind the poor progress and urgency due to the impending wedding in the family, biopsy of the lymph nodes was advised, two lymph nodes were taken out and sent for histopathology.
One came as TB and the other came as Lymphoma. The patient, his family and I were rudely shaken. I had the unpleasant duty to explain what had happened and why the patient was not responding on expected lines. They were in no mood to understan*; their confident world had collapsed and they held me responsible for the dela* in diagnosis and the discussion was bitter and acrimonious.
He did not come back to see me, but I learnt later that despite chemotherapy, he passed away in three months’ time.
With all the exp*rience of 40 *ears and having special interest in TB [having successfully treated more than 500 patients] this was my fate, and it took a long time to recover from this experience
Lessons learnt:
In multiple lesions, better to do multiple biopsies.

Never be overconfident, rethink the diagnosis at eve*y visit particularly when there is no expected response.
Never ever give any guaranteed assurance about recovery.
Readers should keep in mind that tuberculosis can be an opportunistic infection with any pre-existing primary illness such as HIV, malignancy, auto-immune disease, patients on immunosuppressive therapy (like steroids, anti-cancer therapy)
*y reading this experience, one will realize what a slippery slope we occasionally tread in our patient management. Patients are ignorant and most of them have no knowledge and they entirely depend on us and trust us to do the best. In this case, though the initial diagnosis of Tuberculosis was correct, valuable time was lost as the coexisting cancer was missed. One can argue that I cannot be blamed for presuming the abdominal nodes to be one of T* only *ased on USG findings and getting a repeat biops* done when there was no clinical response to treatment. But then the question arises when faced with multiple nodes, especially in an area prone to malignancy, should one routinely get multiple biopsies from different parts?
I would value readers opinion.
Dr.S.Subraman*am
Family Physician.
email: subbusarof@yahoo.com
22

Are you prepared to respond to a medic*l emergency?
One night Dr Ashoojit Kaur Anand got a call from a neighbour asking her to come and see her dad who was not breathing following a sudden choke while drinking water. Dr Ashoojit and I rushed to her flat.
We noticed him on the sofa with no pulse. We put him on the floor and started CPR and asked her to call 108. We checked hi* pupils and found no reaction to light. We s*cured an IV line start*d and started IV fluid. We also administered Inj Adrenaline. In between we checked carotid pulse. No carotid pul*e wa* felt, tongue and lips were b*uish in color. Ambulance took 45 min to arrive while we continued CPR. Ambulance personnel said. He knows only BLS and did not have adequate knowledge of emergency drugs. The ambulance was also not equipped with emergency kits, drugs, or Ambu bag. He was then shifted in the ambulance was taken to the hospital despite having no hope.
Lesson learned-
-
1. First call should go to ambulance then to others.
-
2. All the doctors should have a kit with necessary equipment for emergency situations containing IV Cannula, e*ergency drugs, Ambu bag, IV fluids etc. (as shown in the figure)
-
3. Everyone should know how to perform CPR including lay people.
-
4. Immediate decision making and on the spot *ction is important.
-
5. The problem of delayed arrival of ambulance needs to be addressed*
-
6. Ambulance should be well equipped with all emergency medicines and also an Ambu bag.
-
7. The family members need to be counselled as to the need or otherwise of shifting the patient to the hospital.
-
8. We need to conduct BLS sessions (as it is par* of primary care health) at schools colleges, companies, gym center, clubs and even in apartment blocks.
Dr Praneeth Pillala and Dr Ashoojit Kaur Anand
PCMH Restore Health, Bangalore

Photo credits: Col (Dr.) Mohan Kubendra
23

Masala
Attacks of sophistication
After many years of practice as a family physician, while I continue to learn daily, there is not much that leaves me befuddled
Recently, I had a new patient walk in and say with an air of gravity, ‘Doctor, I keep g*tting attacks of sophistication in my chest and my cousin said you’re an expert in this’ while pointing to the middle of her ample chest. It made me curious. I had not come across “attacks of sophistication” as the presenting complaint *efore. ‘They come and attacks, I cannot work, I *eel my legs arms die, I shiver and shake and I no get sleep’ she continued’.
It was only then that I realized that by ‘attacks of sophistication’, she meant suffocation!
24


25


26
