

AFPI KARNATAKA QUARTERLY NEWSLETTER
President’s Letter
Dear readers
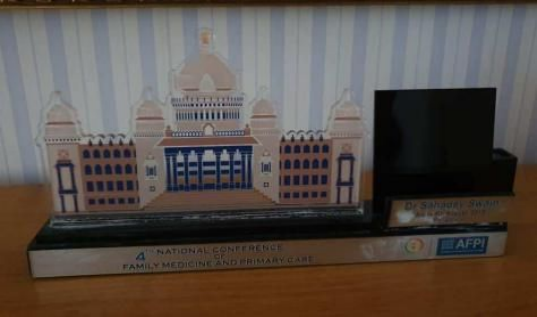
I have mixed emotions as I write this president’s column prob*bly for the last time with the newly elected executive committee ready to take guard *n a few weeks’ time. Ironically the most challenging task of hosting the biggest academic event FMPC 2019 was successfully accomplished in the last quarter by the outgoing team with the support of the emerging leaders from the new committee. Re*ponse to the 4th National conference of Family Medicine & Primary Care 2019 was indeed overwhelming with more than *00 delegates attending the Preconference satellite CMEs, Young Physicians conclave and the main conference at IISc Bengaluru. In my personal opinion the conference has been successful in many ways- in bringing a sense of pride & belongingness to the fraternity, in inspiring & preparing the young Family Physicians to embrace the pleasure & challenges of a career in primary care and in compelling the policy makers & other stakeholders to take note of the mission & the work of the academy. The event had something interesting for everyone to learn from training to practice innovations to technology and research in the field of Family Medicine. A remark from a young resident sums up the impressions *arried by the delegates from the event. He writes I quote “I guess the understanding of the fact that 'this is a conference with it's heart at the Right Place' has been brilliantly portrayed” unquote. For the state chapter emergence of some highly energetic young leaders has been a big positive from this event. As the *rganizing chairperson I wish to place on record my sincere gratitude to each and everyone involved in the success of FMPC-2019.
I am deeply honored and privileged to have served as President state chapter for nearly five years and I relinquish with a great sense of *atisfaction and accomplishment. It has been an incredible journey. I have truly enjoyed getting to know so many of you over the years as we worked together to accomplish the goals I had set for my tenure as the president. I am fortunate that together we could accomplish many of those goals and confident that the newly elected team will complete the unfulfilled tasks and take the state chapter to a greater height. That will only be possible with teamwork *nd continued support from each one of you as the journey will not be without new challenges. No matter what position I hold you can always count on me and I’ll try my best to contribute to the growth of Family Medicine and AFPI.


Lastly, my sincere thanks to the editorial of this Newsletter for creating this platform and giving me an opportunity to share my thoughts. An e*rnest request to all readers to actively contribute in complementing the efforts of the editorial team.
Warm Regards
Col (Dr.) Mohan Kubendra President
AFPI Karnataka
Letter from the president elect
Dear Friends
It is with great privilege and a little skepticism that I am stepping into the shoes of someone who led AFPI Karnataka to such great heights. The suc*ess of FMPC 2019 is just one example of the hard work and perseverance with which the entire team heade* b* Dr Mohan had put forth. We thank all those who supported u* in this endeavor – directly and indirectly. An event of this magnitude could not be done without the dedication of all my team and I express my sincere gratitude to each and every member of the organizing committee for being there and doing their best.
FMPC gave us a lot of insights- that family physicians are respected by doctors all over the world, that we can be our own inspiration, that the policy makers are still unaware of this great specialty and its future, that many bureaucrats believe family physicians are- and should be the pillars of pri*ary care in ou* country… and much more! The conference app, souvenir, theme, inspirat*on room and unique scientific sessions were appreciated by all the national and intern*tional delegates who attended. It also made all of us a real extended family with lots of fun time and anxious moments throughout the journey.
The next few months will *opefull* see an added effort to educate fresh graduates and medical students about this specialty, addition of more seats for the same by Rajiv Gandhi University, NBE, AIIMS & man* other universities, and some good interaction with policy makers in Karnataka to involve family medicine specialists in primary health centers. We urge all of you to come forward and be a part of this tough yet exciting journey that we are taking forward.
This newsletter has some glimpses of the mega event with lot more of knowledge and updates. Happy reading ….
Warm regards
Dr Swapna Bhaskar
President elect – AFPI Karnataka
2

Editorial Note
Conference and after
The recently concluded national conference revealed incre*sing interest in the discipline of family medicine as a career. The delega*es who numbered nearly 800 were mostly young and this from our view is good augury for the future of health care in this country. The fl*p side is that most delegates were fr*m the unorganized sector, in the sense, except for few like CMC Vellore, they were mostly free lancers or from NGOs.
While it’s true that private medical care is important, it cannot deliver universal health care for the country covering all strata of society. It has to come from the health systems being operated by the government. Private medical c*lleges will, as I see it will be reluctant to begin departments of family medicine as from their point of view there is poor money generation. Therefore, at least initially it has to be the government institutions who should take the lead.
It took some effort and persuasion to mobilize some participation from the *overnment. Even here the numbers were only a small percentage of the total.
But the interest shown by the young medical graduates to wards opting for family medicine as a career was truly heartening and if the government and health universities play their part, in the course of time, medical students will opt for this career in increasing numbers. This is good for the country’s health.
New editorial team
Next issue onwards, you will have a new team of editors. We have run this newsletter cum journal for three years and we felt it is time that the new and younger team takes over. I am sure unde* their leadership the newsletter will be richer in content and will also reach a greater number of readers. We welcome Dr Akshay S Dinesh and his team and wish them all the best.
Lastly we would like to place on record the support that we have received from our president and his team in our effort to make this newsletter an effective mouth piece of AFPI Karnantaka.
3
NAMMA BENGALURU: FMPC 2019
Some personal reflections
Dr Sahadev Swain - sahadevswain@hotmail.com
The date was set for the conference about 2 years ago. The month of August is the rainy season in I*dia. We don’t like visiting India at this time. The dry heat in Delhi, rain, and humidity in Odisha and flooding in Mumbai are to be expected at this time. The traffic in Bangalore gets worse in rain. However, my wife and I have always attended FMPC in the past and this one was not to be an exception. However, a health scare to my own health made the journey almost on the verge of cancellation. But my determination and some sort of stubbornness resu*ted in the cancellation of the cancellation and we set off!
We actually reached the town two days ahead of the conference. We are overwhelmed by the hospitality extended to us by our host who are parents of a close friend!

We went around Bangalore mainly using public conveyance like metro to places like Lalbagh and ISKCON Temple. Not

to forget the dining experience at MTR! So, we were already initiated to the concept “Namma Bengaluru”!
Bangalore city, unlike other Indian cities, has a unique feel. The newer technology nicely blends with the traditi*nal streets in the city.
As per the conference, as international faculty, has also shown exceptional hospitality in terms of accommodation, travel, and food to us. Thank you, the organizing committee. My wife and I are extremely grateful!

A record number of (about 800) of delegates attended the conference. There was something for everybody. The 3 satellite postgraduate sessions were oversubscribed.
4

The conference was inaugurated by a lineup of dignitaries .it l*oked colorful. The guests included the president of the national board of examination, Dr. Abhijit, an eminent cardiothoracic surgeon, the Vice-Chancellor of Rajiv Gandhi University. The Mayoress of Bangalore impressed all of us all with her simplicity. Although I did not understand fully her inaugural speech in Kannada what I sensed that she was intrigued by the concept of family Physicians. It would be nice to have one doctor ( Kutumba Vydya) to go for all the need of your whole family rather than visiting the umpteen number of specialist separately. The inaugural function is always prolonged than planned. It was heartening to see the groups like AFPI Kerala and individuals being recognized for their outstanding work. I will particularly mention Dr. D N Sharma memorial prize for the best thesis award that I had instituted in the memory of the general practitioner of my village and my first role model.


What I was also particularly pleased about the release of the book we have been trying to edit with for a while. This was actually one of the reasons why I did not want to cancel my journey the last moment.
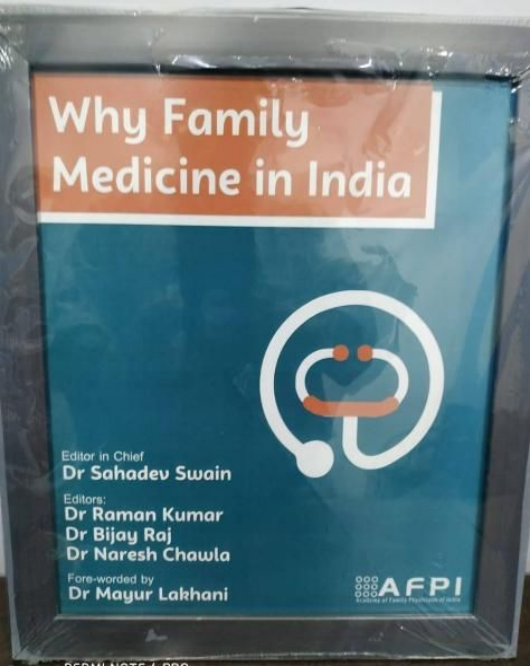
The editing the book has brought me in contact with many family Physicians. This has also given me a chance to look at the development of family medicine in India*
The FMPCs also give me a chance to look at the development of Family Medicine in India up close. I
5
distinctly remember there was hardly 30 people around the table in the gener*l body meeting 1 st FMPC at Delhi. Slowly the number and the stature of the leaders have grown over the period of time. So also the number of delegates attending the conference. It is always heartening to see the growth of family Physicians in India. The young doctors who used to be volunteers as residents are now holding faculty positions and conducting the meetings and sharing sessions effectively and efficiently. Certainly, something very exciting to observe!

What was particularly heartening to see the democratically elected executive of the AFPI and the financial transparency of other organization in the form of audited accounts in the general body meeting of this year.

In organizing conferences large-scale like this money is always a worry. The FMPC conferences are unique in a way they are not sponsored by large multinational pharmaceutical companies. However, the organizers informed that all the stalls were sold easing the financial pressure. I’m *ure it is

only possibl* but the negotiation power and influence of the organizers.
The conference was a feast of scientific programs. The scientific committee is the grandmaster of the whole orchestra. I’m sure they have to invite, design and select the speakers and the sessions to make the learning experience of the delegates enjoyable. Many sleepless *ights for peer-reviewing the abstracts as well. In addition, a lot of struggling and juggling of the sessions and the rooms available.
I was impressed with the customized mementos.
There were inspirational books as a present to the spea*ers and unique concept indeed o*ganizers have certainly been very thoughtful.
6
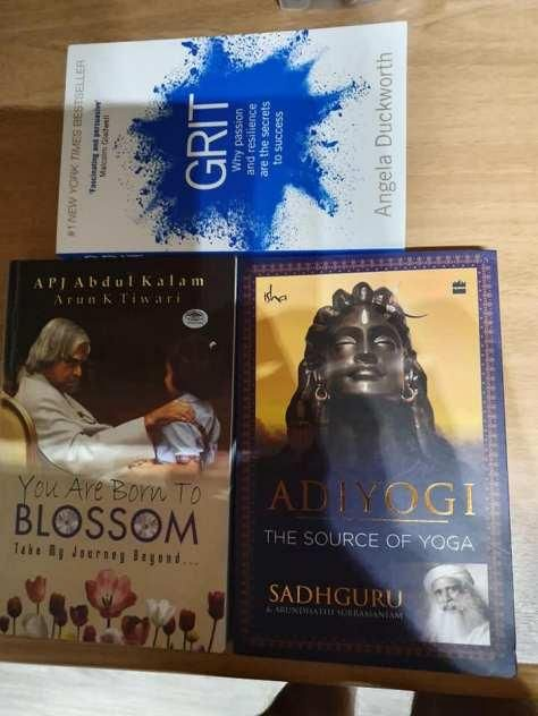
The material of the bags is of special note!

The keynote speakers chosen were inspirational. Dr. Rao raised the important issue of stress among the doctor’s and

advised to utilize customized methods to suit individual circumstances from sports, exercise or meditation for de-stressing. He also advised being mindful of the emotions of the patients that are transmitted to their physicians ,Dr. Pandya highlighted the importance of cooperation between primary care and secondary care Physicians. He recommended the importance of creating group Practices for family Physicians. I thought his interpretation of artwork f*om the Tate Museum “the doctor” was very interesting.
The orthopedic surgeon demonstrated state-of-the-art work being done at t*e Sparsh hospital. The NBE president promised an additional 500 seats for family medicine. The Vice-c*ancellor of the Rajiv Gandhi University promised to write to all the medical colleges in the st*te of Karnataka to start family medicine departments.
Dr. Shailendra Kumar cautioned the audience about the inappropriate use of technology and particularly not to use technology in the wrong order. For example not to order CT scan first without talking or examining the patients.in that case, one will be doing a disservice to the patient and will be chasing” incidentaloma” s. He also highlighted that unique selling points of family medicine are: first Co ntact, continuity, comprehensiveness, coor*ination and contextual care. He also brought to our attention the unsolve* problem of abusing technology for the life support of terminally ill patients AFPI special interest group may be called upon to solve this important complex ethical problems. Dr. Prasad highlighted t*e importance of co-production value of the patients as partne*s as opposed to evidence-based medicine. I can paraphrase *his we should be routinely asking our patients; “what is the matter wit* them” and” what *eally matters to them?” he ended saying family medicine has a responsibility to save medicine. That way, I’ve always believed this is more relevant in the Indian context.
Our very own AFPI president Ram*n Kumar in his presidential speech made a very emoti**al appeal. He brought home that the violence against the doctors is like
shoot*ng the messengers for the bad news. The public is expressing resentment against the poli*icians for poor investment in the government health sector in India. He
highlighted that just like “roti, kapada* and makan“
an essential commodity for each citizen.
,
*ealth is
As per my own sessions, the release of the book “why family medicine in India” what a proud moment for me. The VC of RG University and the president of the National Board of examination w*re present at the time of th* re*ease of the
7
book. The book seems *o have aroused a widespread interest. This also allowed me to be the part the” meet the authors” session in the inspiration room. The session was conducted well, with two other authors. Dr. Rao and Dr. Smruti. Dr. Smruti conducted the interviews watch contract in a “10-minute consultation Style”. The authors discussed what made them write the book, what audience they had in mind. It was highlighted that it is always difficult to find a publisher.
What I found interesting and unique this time was the conference app. Keeping up with the theme of the conference” Technology and innovation” it was first *or the FMPC 2019. However, my phone is registered in the UK, and when I want on to download the app it said that this app is not available in your country. Therefore, as a chair, I had to rely on my co-chairs to interact with th* audience.
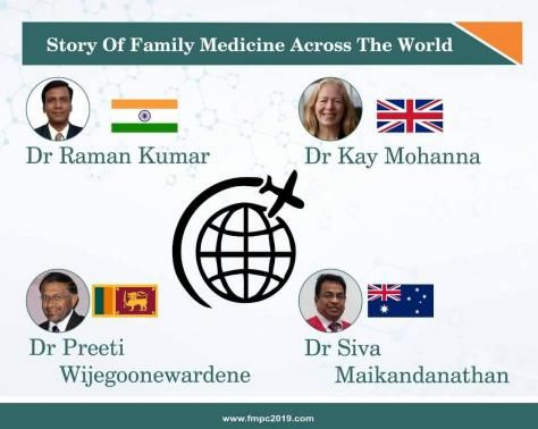
It was lovely to hear the story of family medicine from different parts of the world. It is the contin*ity of care and the mutual trust b*tween the doctor and the patient appeared to be the common theme. While there is a commonality between the UK and Australia the development of family medicine appears t* be patchy in the south Asian countries. However, Sri Lanka and Nepal appear to be further in the journey than India. It was loud and clear that we can all learn from each other.
I also conducted a session on mindfulness for Family Physicians. My co-facilitator was an experienced family physician fr*m Tata health. It is a well-known fact that stress among Physicians is very high, so also the suicide rate among doctors. Mindfulness is one of the evidence-based practices

known to reduce stress. Mindfulness-based therapies now an accepted method of treatment for anxiety and depression.

I felt the session was interactive and there was a lot of participants participation

I sincerely hope that Tata Health will take it up for the Professionals.
The conference is not only about the events that happen in the confinement of the halls. it is also about what happens over a
8
cup of tea and coffee. Therefore it is very important to build up coffee time to the program.
While my wife was enjoying an important session in the inspiration room about how to set up your own practice we literally cornered Dr. Rao to write his biological account. I also established a connection with some family Physicians.


I’ve now been i*vited to attend the next FMPC and the WONCA rural conference in Dhaka. Professor Sasidharan has promised to come to Odisha so that we can together convince the Chief Minister of Odisha to create Kerala model of family centers in O*isha.
Because of some of my own health problems my travel was going to be canceled. But for my stubbornness and m* wife’s cooperation, otherwise, I would have m*ssed *ll the fun! Looking for a bright future *or the family medicine in India and globally I sign off!
9

Experience
A Medical Camp and House Visits organized by PROJECT SETU – A Report Dr Dr. Roshni Jhan Ganguly - roshnijhan@hotmail.com
A free medical camp and house visits was organiz*d by PROJECT SETU in association wit* Academy of Family Physicians of India and AFPI Kerala Chapter in Koothattukulam, E*nakulam, Kerala.
Dr. Shobha Prabhakar, Dr. Indu Rajeev, Dr. Resmi Menon volunte*red to be part of the medical camp offering their full support to Dr. Roshni Jhan Gang*ly (Project Founder and Director) to execute the project. Amanakara sri Bharatha Swami Kshethram Devaswam Trust committee supported us by making all necessary arrangements and providing support staff.
The Gen*ral health screening was attended by 100 people. All adults were screened for Hypertension and Diabetes and follow up was done for the same. Other general problems like Anemia, Worm infestation, hemorrhoids etc. were also addressed. Complaints regarding vision and other ophthalmic complaints were referred to a nearby hospital. Patients with altered findings and poor adherence to the old treatment were referred to higher centres for further need. Dr.Sangeetha *ho
Why I choose Health Equity Research?
Dr Swathi S Balachandra - swathisb01@gmail.com
I app*ied to attend a workshop on *utting edge research on health inequalities: Concepts & methods *t Bangalore that’s being held from 25th-29th of November 2019.
One of the questions was- Please share a brief (up to 750 words) describing the reasons for your interest in health inequities research and what you expect to learn from the workshop.
I with much enthusiasm, wrote down the following response only to realize later that the actual limit is 795 characters and had to pare down to the acceptable limit.
But it was a happy mistake and I found it a reflective exercise on how I've evolved and the directions I'm currently taking and I felt it is worth sharing this in the newsletter.
What follows is my response.
practices in Chazhikattu hospital, Thodupuzha and also t*ok part in the camp would take care of the follow ups. In this way we also created a Fam*ly Physicians network to maintain the continuity of care.
Dr. Shobha Prabhakar and Dr. Roshni Jhan Ganguly also did home visits to understand the socioeconomic conditions and its impact on the bi*psychosocial di*gnosis. This truly gave an insight to their living conditions and its effect on their health problems and quality of life. We collected all the data in a comprehensive assessment sheet which would be used for future research purpos*s. We realized that awareness, adequate finances and timely intervention were key to good health.
It was overall a very satisfactory camp with an overwhelming response. This is just the beginning and we will be continuing this activity on a regular basis in the same place and across India.
I’m a Primary Health Care Clinician and Researcher who believes in Health Equity and quality health care for all and I have the ability and the passion to learn anything that facilitates me to take steps towards this purpose.
From my Undergraduate training days, I’ve been appalled by the fact that the quality and access to health care is very different for different communities and cannot be taken for granted, though I believe health care to be a basic human right. I started following lectures online thr*ugh cour*era on global health and research methods. One of the main resources that hel*ed me gain a better perspective on health inequities research is through the Webinars “Equilogues” conducted in 2017. That is when I was exposed to interesting qualitative research methods and its importance in health research. This encouraged me to do a qualitative research for my thesis in my fellowship. Since then, I’ve always leaned
10
towards research that comprises of systems thinking and involves mixed methods.
During my fellowship at SVYM [Swami Vivekananda Youth Movement], I learnt that one can be both a practicing doctor and be active in public health at the same time if the right attitude and lens is used. This is also the place where I appreciated the role of community engagement and participation.
I believe that quality and responsive primary health care can actually contribute to a large extent in dealing with the problem of health inequity. Currently a huge gap exists between what the health needs and expectations are of various communities are and what the health care system is able to deliver. The gaps are not just a* the service delivery level or infrastructure and budget level, but at understanding of different *ommunities, capacity level, trust in the health care system, empathy, holistic care approach, multidisciplinary approach, person centered care etc. This is complicated by various societal hierarchies, *ocial stigma, and economic disadvantages.
With the above background, currently I have started working with the Women in Sex work and Trans*ender communities in Ban*alore to understand their health needs and h*w best a navigational support system can help in improving the access to primary care for these communities. This is a proposal which I and my colleague* submitted to Grand Challenges Canada Bold ideas Big impact in September 2018. This includes building an app, a community leadership and a network of primary care providers who are responsive to the needs of these *ommunities. We are currently developing the study and yet to roll it out. I have attended a few workshops

at the Institute of Public Health and have been more and more interested in participatory research and methods.
I, being a member of AFPI (Academy of Family Physicians of India), with my other colleagues are also building a Primary health care movement of doctors with the attitude of Primary Health Care as a holistic concept to reach out to the public through videos, newsletters to bridge this communication gap between healthcare professionals and society in general. Over the next few years, I also intend to pursue a PhD in public hea*th which would be related to health equity research.
I will benefit immensely from this workshop on cutting e*ge research on health inequalities: Concepts & methods for the above-mentioned project and work.
Through the workshop I intend to
-
● Strengthen my knowledge in various methods including frameworks in health inequities research.
-
● Understand how to wear the lens of health inequities in every stage of research from framing question to drawing inferences.
-
● Simultaneously try to understand at a deeper level through discussions, the v*rious methods applicable to my current project and work.
-
● Connect with a diverse group of people from the various universities working towards health equity and learn from them.
-
● Get a bigger view of the landscape of Health inequities research in India and globally which would help me shape and get id*as for my PhD program
11
Gleanings
The immun*therapy prize!
The idea of stimulating the immune system to recognize and destroy cancer is more than 100 years old, but the development of effective immunotherapies has been challenging. The breakthrough came from the work of James Allison and colleagues, who elucidated that regulatory mechanisms fine tune the immune responses to ensure maximal efficacy a*ainst infected or abnormal cells without harming healthy tissues. Allison’s group and others showed that CD28 and CTLA-A4 are key molecules with opposite roles in the regulation of CD8 T cells, the primary population of immune cells responsible for recognizing and killing cancer cells and infected cells: CD28 enhances T cell activation, whereas CTLA-4 acts as an inhibitory receptor, also called an immune checkpoint, abrogating T cell activation. James Allison went on to postulate that immune responses against cancer cells with high resemblance to normal cells may be suppressed by CTLA-4. He tested his hypothesis in preclinical tumor models and showed that inhibiting this pathway with a blocking antibody against CTLA-4 induces tumor regression by unleashing the antitumor immune response. These results led to the development of ipilimumab, a monoclonal antibody against human CTLA-4, for the treatment of cancer. It was the first immunotherapy to demonstrate survival benefit for patients with metastatic melanoma and was approved by the U.S. Food and Drug Administration in 2011. The remarkable success of ipilimumab laid the foundation for the development of other immunotherap*es and, specifically, of drugs that target other immune checkpoints. Since then, antibodies blocking the immune checkpoint PD-1 or its ligand PD-L1 have been developed and commercialized. Remarkable features of these immunotherapeutic agents include their relatively good tolerability and the durability of the responses, which results from induction of long-term memory immunity that can control tumors in patients for years. However, the current immunotherapies targeting immune checkpoints have limitations. Only a relatively small fraction of cancer patients benefit from the current treatment. Additional immune check*oints that may also be involved in suppressing tumor immunity have been identified, some of which are now being evaluated in clinical trials. The

challenge is that multiple pathways likely suppress tumor immunity, and combination therapy will be required to improve responses in a broader number *f patients. For example, the blockade of both CTLA-4 and PD-1 pathways is more effec*ive than the blockade of either path*ay alone. To improve immunotherapy treatments, in-depth immune monitoring of cancer patients is critical to provide further insights into the basic mechanisms that regulate tumor immunity and to shed light on the impact of immune intervention on tumor immunity. This information will help select patie*ts who are more likely to respond to treatment, allow the design of rational combination therapies that provide optimal benefit to patients, and also help identify new targets for immunotherapy.
James Allison’s work has provided insights into key mechanisms that regulate immune responses and was the foundation for the development of the transformative new class of immunotherapy agents, and for this, he received the 2018 Nobel Prize in Physiology/Medicine along with his Japanese counterpart - Tasuku Honjo.
This article is a slightly modified version of the editorial that was originally authored by Lélia Delamarre and appeared in Science Advances under a CC BY-NC license*
Please check o*t this detailed article about him, his work and the timeline of events that led him to this discovery :
12
Case Report
When in doubt, it could still be Gout Dr BC Rao - badakere.rao@gmail.com
History and Examinatio*:
Mrs. T, a 62 year old lady presented with complaints of acut* pain and throbbing in her left big toe which was of a day’s duration. There was no history of fever, fall/trauma. This was the first time she had developed such a swelling and it was not associated with swelling of any other joints.
Re*arding her other medical conditions, she is diagnosed with asthma and is under good control with bronchodilators. She doesn’t have diabetes, hypertension, or any other illness. She doesn’t consume alcohol, nor smokes and her diet is vegetarian.
There is no such episodes noted by her in her family up until date.
On examination, she is thin built, with normal temperature, pulse *nd BP. Local examination revealed swollen, erythematous and exquisitely tender metatarso phalangeal joint of the left big toe as seen in the photo 1. Mobility was severely restricted due to exc*uciating pain. Rest of the joints were normal and other systemic examination revealed nothing unusual.

Photo 1

Management
A diagnosis of acute gout attack was made and she was put on colchicine 0.5 mg four times a day. She was asked to come for review after three days with a blood uric acid level report
She followed the advice and review*d after 3 days. She was much better with 90% pain reduction and appreciable reduction in swelling and erythema as shown in photo 2. Her uric acid levels were 4.5mg/dl. It was well within normal range and the same (4.5 m*/dl) two years ago when she was tested as a part of routine health check.
Colchicine tablets were continued for a month and stopped. She recovered from the episode and has no swelling and pain. Since this was the first *pisode no further medications were prescribed.

Photo 2
Discus*ion
The clin*cal syndrome of gout arises from depo*ition of monosodium urate crystals in joints, where they cause an inflammatory response while the same deposition in soft tissue *o*sn’t cause such inflammatory res*onse. The incidence of gout increases with age, more so in post-menopausal women. Inherited factors play a major role. Common presentation of gout is an acute monoarthritis of
13
rapid onset, often waking patients from sleep. The most commonly involved joints are the great toe, foot, ankle, knee, wrist, finger, and elbow, possibly because the monosodium urate is more likely to crystallise in cooler parts of the body.
Though there is a correl*tion between raised blood uric acid levels and occurrence of acute gout, the two can exist independently of each other. The risk of a gout attack increases with increasing uric acid levels, but many patients will have attacks with normal le*els of uric acid and some will never have an attack despite very high levels of uric acid who are termed as having “as*mptomatic hyperuricemia”. This means that acute gout can exist with patient having normal uric acid levels. One should not especially look for increased uric acid level during the acute gout attack as the chances of it being normal is clos* to 60%. Also even if the previous uric acid levels are normal, one should not hesitate to make the diagnosis of gout in a patient presenting with classical signs of gout as it is in this case. The rapid response to colchicine further supports the diagnosis.
Serum uric acid values between 3.5 and 7.2 mg/dL in adult males and postmenopausal women and between 2.6 and 6.0 mg/dL in premenopausal women is considered as normal *n many countries.
There are several studies which have shown that varying percentage of patients having norm*l or below normal uric acid values presenting with acute gouty attacks. These are patients who excrete uric acid more than usual in the kidneys called over excreters versus under excreters. The treatment modalities are the same in both.
Treatment of acute gout attack includes NSAIDs, Colchicine. Chronic management to reduce future attacks involve lifestyle changes like dietary modifications like reducing meat/fish, reducing alcohol intake, and weight reduction. Uric acid lowering therapy with agents like xanthine oxidase

inhibitors (XOI) or uricosuric drugs is indicated for patients with recurrent or severe course; the target uric acid value is <6 mg/dL. Long-term treatment should be initiated only after resolution of the acute attack. Patients with asymptomatic hyperuricemia and normal kidney function is not an indication for uric acid lowering therapy.
It is important to note that patients with hyperurice*ia may remain asymptomatic, though there is growing evidence that silent deposition of monosodium urate crystals may occur and lead to early destructive skeletal changes. In addition to this uric acid may also play a pathophysiological role in many "cardio-nephro-metabolic" disorders, which seems to be independent of the deposition of monosodium urate crystals, since it is evident also for serum uric acid concentrations below the saturation point for monosodium urate. Hence the question exists whether the current normal range of uric acid needs revision a*d whether “asymptomatic hyperuricemia” needs active management especially when *here is a higher risk of metabolic syndrome / cardiovascular events.
With inputs by: Dr Swathi S Balachandra
References:
-
1. Underwood M. (2006). Diagnosis and management of gout. BMJ (Clinical research ed.), 332(7553), 1315–1319. doi:10.1136/bmj.332.7553.1315
-
2. Naomi Schlesinger, Josephine M. Norquist et al. Serum Urate During Acute Gout. J Rheumatol 2009;36;1287-1289
-
3. Băd*lescu M, Macovei L et al. Acute gout attack with normal serum uric acid levels. Rev Med Chir Soc Med Nat Iasi. 2014 Oct-Dec;118(4):942-5
-
4. *esideri G, Castaldo G et al. Is it time to revise the normal range of serum uric acid levels? Eur Rev Med Pharmacol Sci. 2014;*8(9):1295-306.
14

An Unusual presentation of Undifferentiated connective tissue disorder
Dr. Shaik Shahnaz *arveen, Dr Swapna Bhaskar, Dr Chethana Dharmapalaiah - swapnabhaskar305@gmai.com
Introduction Connective Tissue Disorder was made and Rheumatologist
The term undifferentiated connective t*ssu* disease (UCTD) is used to define clinical entities characterized by features suggestive of CTD which do not meet the classification criteria of the American College of Rheumatology for a specific single disease, such as systemic lupus erythematosus, systemic sclerosis, polymyositis / dermatomyositis, and Sjögren's syndrome. (1-4)
As only a few reports have described of UCTD the natural history still remains unknown and unpredictable but it is a type of autoimmune disease. Symptoms of UCTD vary, but more common symptoms include Raynaud phenomenon, arthritis, joint pain, fever, and symptoms involving the mucous membranes and skin such as dryness in the eyes and mouth, ulcers in the mouth and photosensitivity. (5)
Case report
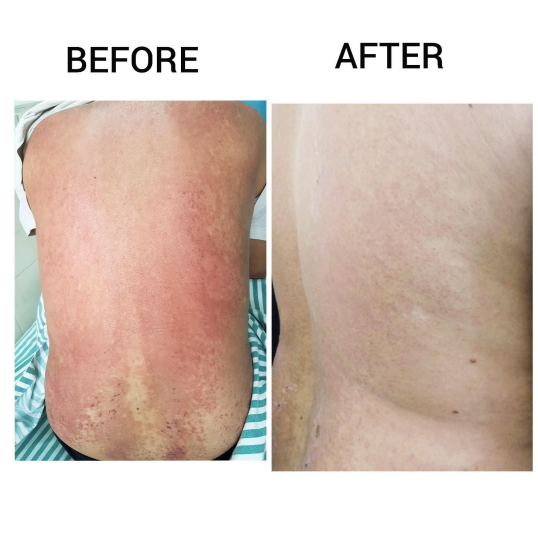
A 42 year old male presented to the Family medicine opd with chief complaints o* low grade fever since 1 month duration, painful ulcers in mouth since 1 month and generalized erythematous rash with ulceration.
According to the patient, who was apparently normal 1 month back w*en he developed fever of low grade without chills and rigors followed by body and joint pains. Later he developed painful ulcers in the mouth and generalized erythematous rashes over his body which was not associated with itching. Patient also had significant weight loss which incapacitated him from work Before visiting this OPD, Patient h*d visited multiple doctors and was investigated extensively, including infectious panel like Dengue, Leptospira and MP antigen which was negative. He received symptomatic treatment but was not completely relieved. Later on a visit to a Dermatologist the patient was started on Dapsone 100mg OD after which he felt better and mild resolution of rashes but the rashes recurred along with high grade fever. No significant past medical or family history nor any history of substance abuse.
General physical examination revealed extensive mucosal ulcerations, generalized erythematous rash over the body, respiratory system examination revealed infrascapular crepts on the right side with normal oxygen saturation on room air. Other systemic examination was normal.The diagnosis of
(Dr Chethana) opinion was sought for the same. Investigations
All the routine investigations like CBC LFT, RFT, SE, RBS were normal. Serology (HIV Elisa) was negative, ESR was 32mm/hr and peripheral smear showed Lymphopenia with relative neutrophilia. Sputum for gram staining showed many pus cells. ANA profile: Ro 52 positivity 3+, C3 C4 com*lement levels were normal.
Treatment
The patient was admitted to the ward and was treated for autoimmune disease with oral steroids and HCQs for which the patient became afebrile and showed tremendous improvement in rashes and mouth ulcers. Patient was discharged after 1 week on HCQs and T. Wysolone and is on a regular fo*lowup on OPD ba*is and currently on tapering doses of steroids and minimal mucosal ulceration and is returning back to his normal life.

15
Discussion
In our case, the initial presentation was fever and generalized rash without itching, but the exact pathology behind any of the presenting symptoms could not be found, even after thorough evaluation of all the symptoms and physical signs and laboratory investigations. But as the suffering of the patient continued, more and more signs and symptoms began to appear which gave clues that a rheumatologic disease could be responsible. In diagnosis and classification of connective tissue diseases, the clustering of symptoms and signs into readily recognizable groupings has an important historic precedence. In some cases when diagnosis of a specific connective tissue disease is not always obvious, this is often referred to as undifferentiate* connective tissue disease (UCTD) [7]. In their early stages, many autoimmune connective tissue diseases (AICTDs) are not cli*ically
|
well |
differentiated |
and |
then |
they |
belong |
to |
UC*D |
(8) group |
|
|
. |
About 50% of UCTDs remain undifferentiated also later in the course and never resemble any specific autoimmune disease with mainstay of treatment being steroids to which the disease responds. (9-11)
Conclusion
Systemic rheumatologic disease can hi*e behind rather non-specific and seemingly unrelated symptoms and signs. We therefore recommend holding a high degree of suspicion in the susceptible individuals, and always consider the

possibility of presence of any autoimmune pathology. But it is always necessary to diagnose early in order to decrease morbidity, and disease related complications.
References:
-
1. Van den Hoogen F, Khanna D, Fransen J, Johnso* SR, Baron M, Tyndall A, M*tucci-Cerinic M, et al. 2013 classification criteria for systemic sclerosis: an American college of rheumatology/European league against rheumatism collaborative initiative. Ann Rheum Dis. 2013;72(11):1747-1755
-
2. Ines L, Silva C, Galindo M, Lopez-Longo FJ, Terroso G, Romao VC, Rua-Figueroa I, et al. Classification of Systemic Lupus Erythematosus: Systemic Lupus International Collaborating Clin*cs Versus American College of Rheumatology Criteria. A Comparative Study of 2,055 Patients From a Real-Life, International Systemic Lupus Erythematosus Cohort. Arthritis Care Res (Hoboken). 2015;67(8):1180-1185.
-
3. Alarcon-Segovia D, Villareal M. Classification and di-agnostic criteria for mixed connective tissue disease. In: Kasu*awa R, Sharp G, editors. Mix. Connect. Tissue Dis. Antinucl. Antibodies. Amsterdam: Elsevier; 198*. p. 33-40.
-
4. Kahn M, *ppelboom T. Syn*rom de Sharp. In: Kahn M, Peltier A, Meyer O, Piette J, editors. Mal. Syst. 3rd ed. Paris: Flammarion; 1991. p. 545-556.
-
5. Sharp GC, Irvin WS, Tan EM, Gould RG, Holman HR. Mixed connective tiss*e disease - an apparently distinct rheumatic disease syndrome associated with a specific antibody to an extractable nuclear antigen (ENA). Am J Med. 1972;52(2):148-159.
-
6. R Kasukawa, T Tojo, S Miyawaki. Preliminary diagnos-tic criteria for classification of mixed connective tissue disease. In: Kasukawa R, Sharp G, editors. Mix. Connect. Tissue Dis. Antinucl. Antibod*es. Amsterdam: Elsevier; 1987. p. 41-47.
-
7. LeRoy EC, Maricq HR, Kahaleh MB. Undifferenti-ated connective tissue syndromes. Arthritis Rheum. 1980;23(3):341-343.
-
8. Alarcon-Segovia D. Scleroderma: From Morphea to Sys-temic Sclerosis-The Clinical AspectMixed *onnective tissue disease and overlap s*ndromes. Clin Dermatol. 1994;12:309-316
-
9. Maria Dall'era, David Wofsy. Systemic Lupus Erythro-matosus. In: Gary S. Firestein, R Budd, SE Gabriel, JR O'Dell, IB McInnes, editors. Kelleys Textb. Rheumatol. 9th ed. Philadelphia, PA: Elsevier/Saunders; 2013. p. 1284.
16
-
10. Pott Junior H, Ama*e Neto A, Teixeira MA, Provenza JR. Ascites due to lupus peritonitis: a rare form of on-set of systemic lupus erythematosus. Rev Bras Reumatol. 2012;52(1):116-119.
Shared Decision Making
On the 16th and 17th September at the University of Chicago Centre in Delhi, a session titled "Progressing with Partnerships : Shared Decision Making among Vulnerable Groups" was org*nised by the Buksbaum Institute for Clinical Excellence, University of Chicago, Medical Humanities group, UCMS, and Manipal Academy for higher education.
It piqued my curiosity. I am a doctor working for comprehensive care for people with genetic diseases who never heard of such a concept in the patriarchal medical world. The event with its diversity of concepts that were covered, exceeded my expectations. Although I was overwhelmed by the *ich talk*, I shall try to do justice it and write it in the best way I can and remember.
The concept of “Shared Decision Making” was described in the first session by Dr Sa*endra Singh, a physiologist by profession, and a renowned Disability activist. He put across that in the Competency based Curriculum designed by medical council *f India, disabilities were not an explicit part. Some time back, the necessary stakeholders gathered and a list of disability competencies were shared and were later inco*porated and arranged according to the 5 roles of an Indian Medical Graduate. Some of them are advocating social inclusion for people with disabilities, awareness of a range of assistive de*ices, encouraging research on prevalence and management of disabilities.
A key feature which strikes *s that an ordinary
doctor can't be
equipped with these qualities without under*tanding the
unique needs of the individual with disability.
This is where Shared Decision Making comes along.
A model explained by Dr Satendra as a “Share approach” for s*ared Decision making involves assessing the needs of the patients by actively engaging the patient with the goal of reaching a management plan that *uits them the best.

-
11. Mier A, Weir W. Ascites in systemic lupus erythem*tosus. Ann Rheum Dis. 1985;44(11):778-779.
Dr Monika peek, an inter*al medicine specialist whose main research interest involves patient/provider communication, with an emphasis on shared decision-making (SDM) among racial/ethnic minorities with diabetes, gave a US based perspective of SDM. And she has suffi*ient work to substantiate that shared decision making is the pinnacle of patient centred care. The work in implementing SDM model correlated with positive health indicators, better glycemic control, shorter hospitalizations, fewer malpractice claims.
So if SDM has so much value in it to address health inequity, why does it seem like a novel concept?
Peek explains that existing patient-provider power imbalance, especially where care provideres are white, heterosexual male and are documented citizens of the country, and pati*nts form a sexual/racial minority, both parties involved view each other through the lenses of societal sterotypes, prejudices and normative beliefs. Patients lose the social accountability to demand better healthcare. A provider should be incorporating the three domains of SDM, 1.Information sharing of evidence based reasonable alternative *ncluding no intervention, with risks and benefits, 2. Collaborative deliberation resulting i* preference based decision, 3. Decision making which results from patient values, goals and informed preferences.
Anant Bhan president of th* International Association of Bioethics, critically analysed the factors in Inidan context which thaw patients from being passive recipients in to getting autonomy over *he*r healthcare needs in it* ind*an context where goals of SDM intersect with societal and familial hierarchy, public health services. Dr Bhan highlighted some Indian work. In 2007 a research group studied the efficacy of cow urine therapy on various cancer patients. Illiterate patients were told that they would not survive long, and that cow urine can cure incurable diseases, thus were coerced into consuming cow urine. And other stories about the nonchalant attitude in a casualty for an acid *ttack survivor taken from an expert of the novel "being reshma", made us realise that in India where the dignity of
17
life and death is not often acknowledged as a human right, practicing SDM can be very difficult indeed. He said that there is no SDM tra*ning in India. The new curriculum of MCI introduces SDM as one of the core competencies.
The second session explored SDM among patients with disabiliti*s and chronic pain survivors.
Jo Chopra of Lathika Roy foundation, a NPO that p*ovides care for children with disabilities was reiterating that disable* individuals' needs are not addressed, how society believes they can't take a decision and hence they are are always the third person even in conversations with the practitioners and family regarding their very own health. Doctors can follow a simple method of constantly involving the disabled patie*t into the conversation* with the aim to bring awareness that people with disability need to be accounted for their he*lth rights, even though it's a challenge and may conflict with that of caregivers.
Dr Soumitra Pathrae, a psychiatrist and Director of the Centre for Mental Health Law and Policy, talked about how it is a societal perception that SDM is not easily justified for mental illness. But here comes a model of suppo*ted medical decision which has the same core values as SDM, and it is important because psychiatric patients are conventionall* thought of as lacking capacity to incorporate their will and preference. If psychiatrists focus on medical outcome, it may at times overrule patients wills and preferences. He stressed about giving equal weightage to right to consent vs right to refuse, to note that with the right to refuse there might be decisions which what doctors think are terrible outcomes but they should know that it is a need/value that the patient wants and respect that.
He says better options like psychiatry advanced directives and nominating capacity when someone falls ill are methods that enable working on supported decision making.
Anubha Mahajan, spoke about the immense psychological and economic *istress she faced throughout the diagnostic odyssey of her medical condition - Complex Regional Pain Syndrome and Central Pain Syndrome, which encouraged her to start Chronic Pain India, a trust that raises awareness regardin* medical conditions which are “invisible” to the eye. The lack of management options for such illness among practitioners can perhaps be altered by a shared decision approach to recognize trigger and customise the management of such illness.

In the third session on SDM addressing health disparities among LGBTQIA+ community, Dr Aqsa Shaikh, community health doctor from Hamdard Institute of Medical and Research, Delhi, and Trinetra Haldar Gummaraju, a medical student from KMC, Manipal put *cross the challenges a trans person faces in the patriarchal health system, right from lack of dignity, from the security guard and sexual/emotional/verbal abuse they face w*en they want to avail health services, medical textbooks talking about sodomy as a paraphilia, Government documents being necessary to prove their identity befor they *an access healthservices. Trinetra said she is the one who most ofte* educates her gynecolog*st, endocrinologt, and surgeon about the medical nunances regading transgender health. These stigmas make health seeking behaviour nearly impossible. At the end of this session they gave clarity that the LGBTQIA+ community need to be involved and their leadership alone can make their policies regarding their healthcare better, witho*t which we end up with t*e horrors like the transgender bill of India, which undermines the very own values of the individuals it tries to help.
Haven't we all during our training and practice usually given more attention to the disease and less to the suffering it causes? Doctors and family emphasise safety and medical care, and not a meaningful life with the illness. Pallium India founder Padmashri Dr M R Rajgopal, with their work on palliative care tries to achieve the latter. He made all the participants aware that palliative care is not hospice care, one that terminally ill need, but palliative care should be incorporated at all stages of treatment and prevention right from diagnosis. The relevance of social capital was discussed. A public health system in Kerala is built with trained nurses visiting families with bedridden individuals to assess their needs. When it comes to chronic illness care providers must go beyond the two methods of truth communication which is either blunt truth telling or good intentioned damaging lies, and should engage with the patient to discuss a management plan that suits him on how he wants to live the rest of his life
The second day there was a theatrical form of engagement called theatre of the oppressed. It is a form of community engagement and education. It encouraged participati*n among the audience to take the role of a character that is oppressed in a *lay, and change their narrative, In this particular play, laboured love, the characters were a senior gynecologist who asked the intern to get consent from, a pregnant lady with four girl children for a caesarean section as she has accelerated fetal heart rate, her husband a simple farmer, and her mother in-law who seems to be taking all
18
decisions regarding her daughter in-laws health. The intern tries to get consent from the mother in law for the surgery as the pregnant lady and her husban* refuse to take ownership and sign the consent, but the mother in law won't sign until and unless the intern tells the sex of the child and only if it is male child. The majority audience agreed that intern was the most oppressed and took her role during various timepoints of the play change t*e narrative and get consent for the surgery from the pregnant lady, by trying to make the pregnant women understand or try to get better perspective from son or mother in-law.
For the last session all the participants were split into groups to explore enablers and barriers to practice SDM for vulnerable groups in our settings.

Medical hegemony, lack o* sympathy, lack of funding, Indian family and societal structure and time were the common barriers . Empowering patients and caregivers and allied stakeholders, regular CMEs/new medical curriculum to discuss the social implications of health for minorities, social media and other platforms to raise the primary health care *eeds of vulnerable sections are better enablers as of now.
At the end of this session I felt one missing stakeholder - a family physician is essential to underpin the growth of SDM Methodology in India.
Masala
Kill the patient and get thanked
I was on the phone with the patient's wife. She was asking me if can suggest some medication for her husband who was having severe nasal block and was unable to sleep. I told her the name of an anti histamine and told her that it will give him relief and added for a good measure,'it will also put him to sleep'. She in turn thanked me and wished me goodnight!
Kill the patient?
This morning while examining a patient, I got a phone call. I told the caller that I will call him back after I finish this patient! The patient had the grace not to believe me and stayed put on the examination table.
19
