
Issue: Volume 4, Issue 2
President's Letter
Dr Swapna Bhaskar (President, AFPI Karnataka)
Hello readers!
The world is under the grip of a devastating virus which has made its presence felt in more than 210 countries by now and still counting* COVID 19 has taught us quite a few lessons - that even the most powerful country will succumb, that no age, sex, cast, religion, or economy can escape the fury, that no celebrity, king, PM, or President is infallible, *nd that no one is invincible! The virus is here to stay; our endurance and courage to face it is what matters.
Healthcare workers are the new heroes of the world and family physicians play a pivotal role in containing the pandemic. Hence the recently celebrated world family doctors day had the theme – “Family doctors on the frontl*ne - first in, last out”. One such recognition which came to AFPI Karnataka was from the prestigious Rajiv Gandhi University Of Health Scienc*s, when they
invited us as resource persons to conduct a webinar on “Practice and management of clinics for GPs” on March 27, 2020 as part of their ongoing series.
We take pride in launching the second issue (in volume 4) of our regular newsletter. This edition has a variety of thought provoking and enlightening articles - the uncertainties and challenges of running a private clinic during the pandemic, the art of being a lifelong learner, models of community health in the eyes of a public health MD candidate, reflection on healthcare delivery in India, novel cancer therapy and lots more. Please give our young and energetic team your sincere feedback to improve on what we have been doing since past 4 years.
Happy reading. Stay safe! Stay strong!

Issue: Volume 4, Issue 2
Editorial
Akshay S Di*esh (Primary Care Physician)
The pandemic has left no one untouched. Not unexpectedly, it has disproportionately affected the vulnerable. The dilemmas are also harder for them. Break curfew and walk away from shut down cities towards home, towards family. Stay inside while the savings run dry. Avoid going to hos*ital and risk chronic diseases running out of hand. Close down small establishments. Forgo only source of income. Suffer from intimate partner violence. Take a toll on mental health.
In this edition, there are stories of sustainability and safety and of priorities in running small medical establishments. There are also critiques on the way larger establishments (includ*ng public health system) are run. We also pause to reflect on d*lemmas that a routine consultation can bring. On an optimistic note, there are strategies for lifelong learning, followed by a
schola*ly article on molecular therapy in cancer.
You might have noticed that this issue has been delayed from the usual schedule. We blame the pandemic for that too. The entire world is resolute in getting back on track, and so are we. We learned during the last few weeks the power of modern communication tools. Webinars, videos, group calls, flyers - messages in various forms have been filling that gap created by "social distancing". Personally I feel like this is an opportunity to come together and strengthen this newsletter. If you are reading this, I urge you to send in your suggestions on how we can add more value to the experience. Also send in your contributions - whatever be the form - to our team. Together, let us make this a vibrant platform of ideas and innovation.

Issue: Volume 4, Issue 2
Editorial Note on Opinion Articles
Akshay S Dinesh (Primary Care Physician)
Swathi SB (Primary Care Physician and Researcher)
Dr Sulaiman Sharieff (General Practitioner at Humanity Healthcare and Diagnostics, Tinfactory, Bengaluru)
What is the responsibility of an editorial team when it comes to opinion art*cles? Should *ny kind of opinion be allowed on our newsletter? Should we put disclaime*s stating that we do not endorse opinions stated in such articles? Should we allow publi*ation only opinions that the editorial team agrees with? Should we fact-check statements in such pieces?
The editorial team had an in-depth discussion of the above *uestion* during the preparation of the current issue.
There are broadly two kinds of articles
-
1. Objective articles (eg: academic articles)
-
2. Subjective articles (eg: perspec*ives or opinion pieces)
Articles in the objective category are easy to verify. They are usually accompanied by various references and statements made are falsifiable. It is possible for an editorial team to verify facts and requests corrections on such articles.
But the articles in subjective category are not so straightforward. Disagreements on an opinion are hard to settle. Objectivity is difficult to attain when it comes to broad, ill- defined issues that are commonplace in real world.
Asking the author for citations on a subjective point would be infeasible. If there were citations they wouldn't be "subjective" at the first place. Also, it wo*ld deter submissions from those who aren't very vocal about their opinions. That is not what this place wants to
be. We want our newsletter to be a space for expression.
But what about opinions that are d*sagreeable? What about controversial or harmful positions which we do not want to endorse? Should we welcome them with caveats?
One idea that arose was that we could preface such articles with a disclaimer like this: "This is an opinion piece and the editorial policy is to give a platform for all opinions whether or not we agree. We do not endorse the ideas in this article." This could be suffixed with specific pointers to alternative ideas.
But this could be felt like we are infantilizing our readers. Should the editorial team not let the informed readers make decisions and opinions on their own? Why should we tell them what to think about an article?
Also this leads to antagonizing the author. Some might consider an ou*right rejection fairer than a publication with rejection written all over it. They lose the sense of ownership. They write for the readers and not for an editorial team to judge.
We do believe that an editorial team should have a stance of their own. But how do we express such a stance while avoiding the pitfalls mentioned above?
We arrived at a solution that resolves the conundrum, even though it may bring us more work.
In The Emperor of All Maladies, Dr Siddhartha Mukherjee tells the story of how the US media was required by their federal government to give equal airtime to antismoking messages if they are broadcasting cigarette commercials. This p*ayed a role in combating misinformation regarding smoking at that time and, among other things, led to decrease in consumption of smoking over the years.
Similarly, we plan to balance opinions with counterpoints that a*pear as separate articles. These could be invited articles, republished articles, or even articles written by a member of the editorial team. The fairness doctrine would be fulfilled. The editorial stance would not go unstated. And no opinion has to be rejected. Win for everyone.

Issue: Volume 4, Issue 2
AFPI Karnataka News
*r R L Sankha – the President of Spice Route - SAR visited Bangalore and AFPI hosted a get together for him with young graduates of FM at St Philomena’s Hospital on January 11, 2020. Dr Sankha spoke about Spice Route Movement and its activities and had a fruitful discussion about challenges of general practice in both coun*ries. The session was attended by about 20 doctors and was live streamed on Facebook.
Meet and great with another dignitary Dr Woolever - Director of FM residency, Darmouth, USA occurred on Feb 5, 2020 at Bangalore Baptist Hospital. Many young and experienced family physicians attended it and discussed about FM residency programs and opportunities for family physicians in both countries.
It was a great honor when the VC and team of RGUHS invited AFPI to be the resource provider for conducting a webinar on “training of family physicians in *ractice management”. This hugely successful webinar was live on 27th April 2020 from the
prestigious RGUHS campus. Dr Mohan Kubendra, Dr Roshni Jhanganguly, Dr Swapna Bhaskar and Dr Sowmya B Ramesh spoke on various aspects of COVID-19 in relation to clinical practice including teleconsultation, clinic management and PPEs for family physicians.
AFPI members led another webinar for FPAB members on May 10, 2020 on “Clinic Management and PPEs for the practicing GP during COVID”. Dr Swapna Bhaskar and Dr Sowmya B Ramesh spoke on the topics respectively. The session was attended by over 200 doctors online and well appreciated.
The Public relations team of AFPI has been continuously putting up educational creative flyers on COVID information to the public throughout March and April. The response and acceptance has been overwhelmingly positive.
World family doctors Day (May 19th) was celebrated by releasing a video of patient
testimonials on their family physicians and need for strong primary care in the society. It was really heart*arming to see the wholehearted appreciation of family doctors by the general public and it encourages us to serve our patients even more.
On the special day, there was an exclusive radio program dedicated to family doctors on Big FM.
Due to the pandemic and lockdown, the scheduled CME on “PVD in General Practice” which was to be organized on March 29th had to be postponed indefinitely. The finalized dates will be announced soon.
AFPI published a position paper on "Ensuring continuity of care by small fami*y practices and clinics in the primary care setting during COVID 19 pandemic 2020" which is available online for all family physicians to view.

Issue: Volume 4, Issue 2 Artic*e
Community Health: Stopping the Clock on our Ever- Expanding World
David Warnky (Fullbright-Nehru Student Research Scholar: Institute of Public Health B.Sc. Public Health; M.D. Candidate 2022: University of Kansas)
Introduction
I* the fall of 2011, I was a student *f public health at Kansas State University. I was sitting in a lecture for m* class titled “The Built Environment” when my professor showed a Ted talk from Dan Buetner and
National Geographic. The talk was titled,
“How to live to be 100+.” In this short d*scussion, Mr. Buetner explained the concept of Blue Zones. As reported, Blue Zones are small communities throughout the world where the number of people who live to be 90 and 100 is significantly higher than anywhere *lse in the world. In addition, these areas experience a fraction of the chronic disease present elsew*ere. Essentially, these zones are little havens of health spread throughout the world.
In the video, Mr. Buetner explained that a variety of environmental factors shape this reality. Essentially, these factors fit into four
categories: natural movement, healthy diets, right outlook, and community connected*ess. A* I watched the film, wheels turned in my head. I realized, for the first time, that health might be more related to our environments than th* quality of our healthcare. To an aspiring physician, this was both fascinating and devastating.
The Social Determinants of Health
In the years since, I have continued to pursue an interest in the environmental factors that impact health. Nowadays, I call them the social determinants of health (SDoH). The World Health Organization eloquently defines the SDoH as, “The con*itions in which people are born, grow, live, work and age. These circumstances are shaped by the distribution of money, power and resources at gl*bal, national and local levels. They are most*y responsible for health inequities - the
unfair and avoidable differences in health status seen within and between countries.”
Research has given language to this idea. One study estimates that medical car* was responsible for only 10%–15% of preventable
mortality in the U.S., whi*e another study
suggests that that the SDoH account for between 30-55% of health outcomes in the US. Though controversial, Thomas McKeown’s book, “The Role of Medicine” discusses the idea that overall *ife expectancy has been more greatly impacted by improvement *n living standards than by
modern medical advancement. *rguments
aside, plenty of evidence suggests that health improves as s*cial position r*ses.
An Example
The United States is a prime example of this mismatch. Healthcare spending reaching comprises nearly 17% of the GDP; yet, health outcomes consistently rank among the worst
of the deve*oped nations. In her book, “The
American Health Car* *aradox,” Elizabeth Bradley illustrates that not only does the U.S. spend mor* money on healthcare, but it also spends significantly less money on social
services. T*is is a tragic and costly
imbalance. One need not look far to see the consequences of such discrepancies. Life expec*ancy within a single city can differ by up to 30 years dep*nding on the neighborhood in which one lives.
reality that zip code plays such a role in health and life expectancy is truly tragic.
The
An Economics Issue
I want to remind you that this is most *ertainly an economics iss*e. *or one, healthcare is a billion- or even trillion-dollar industry, and it can occupy a significant portion of a nation’s GDP. Secondly, as we have already discussed in great detail, povert* and inequity are complicated issues. As we examine the *ycle of poverty, we must remind ourselves that community health is a
large player in this equation. Finally, we
must remember that poor health is expensive. A series of papers estimate the annual cost per employee for common lifestyle ri*ks: *moking—$5,800, diabetes—$4,413, obesity —$4,237, and high blood pressure—
$1,077. As globalization continues to
prevail and inequities persist, we must begin to realize the economics of healthcare issues.
The Rural Connection
My original prompt for this discussion was, “The Impact of Globalization on Rural Communities.” I spent a gre*t deal of time considering this line, but ultimately, i* was my experience in some of the rural villages that established the connectio*. In the past, rural communities contained man* of the essential elements for a healthy co*munity.
Regular physical activity was often built in to
the lifestyle. These communities were often
dependent on farming and ranching; travel in and between villages largely depended on walking, and the non-existence of modern appliances demanded increased efforts for
common household chores. The diet was often healthier; many of these communities were likely subsistent. There was no packaged o* fast food. This also encouraged a seasonal and plant-based diet. Moreover, the absence of electricity practically ensured h*althy sleep schedules. People went to bed when it became dark and rose with the sun. These rural communities also ex*erienced a greater level of connectedness. The lifestyle encouraged permanence in a community, reliance on one another, and generosity. Even today, studies suggest tha* rural communities tend to be more generous and social than
urban communities. Spirituality also played
a role. Evidence suggests that people who attend regular spiritual gatherings actually experience decreased levels of mortality in
longitudinal studies. For one reason or
another, rural communities are often more
spiritual than urban comm*nities. For these
reasons and m*re, the tra*itional rural lifestyle actually serves as a great model for community health.
Admittedly, in an effort to highlight the positives, I have overlooked the problems of drought, disease, and violence that were undoubtedly also issues in these communities. I simply wanted to highlight the lifestyle pattern that presented so many positive features.
The Impact of Globalization
By now, the co*cept of globalization has been adequately introduced. While I have almost nothing to add to this discussion, I would like to suggest that globalization is at least, in
part, responsible for our *ransition from healthy communities to the current situation. I will list a few examples. The first of these issues is job insecurity: local farmers competing with land-rich nations, local craftsmen competing with production lines, and local labor competing with population- rich nations. A resulting is*ue of this insecurity has been migra*ion. Initially, this seemed like a positive outcome, but many are beginning to reco*nize the detriments of losing family structure and cultural identity. In additi*n, the increasing “Westernization”of society threatens traditional, cultural, *nd spiritual values. The industrial revolution has marked a major shift from active work to sedentary lifestyles, and the increasing availability of fast and packaged foods continues to diminish homemade, plan*-based diets. While globalization has resulted in many positive outcomes, its impact on the health of our communities is certainly worth noting.
The Role of Primary Care
The current circumstances beg the question, “Where do we go from here?” I believe that one solution is the integration of these social issues into the healthcare sector. Tragically, the healthcare sector is more medicine than it is health. Social issues must become the concerns of the healthcare fi*ld. At my home institution, Kansas University Medical Center, the department of family medic*ne is beginning to screen f*r these social issues. When patients come to the clinic they are gi*en the opportunity to answer questions like the following: are you worried that you
may not have stable housing, did you skip medication to save money, did you ever eat less because there wasn’t enough money for food, and do you ever feel that you lack companionship? To date, nearly 65,000 unique patients have been screened for these issues; the leading concerns in this population se*m to be healthcare costs, access to food, medicine affordability, and social isolation.
Social Isolation
While screening was a good first step, the next logical action is to identify effective interventions for social issues. More importantly, what help could be offered from a primary care clinic? At the University of Kansas, Dr. Jennifer Woodward, Megan Murray, and I partnered with patients to explore creative solutions. The team decided to investigate the problem of social isolation. Studies suggest that nearly 7.7 million older
adults are socially isolated in the U.S.; other
research states that nearly half of all older
adults are isolated in India. Even more
concerning is the current evidence that indicates lack of relationships is a stronger risk factor for mortality than that of obesity. This quality improvement project focused on assessing the quality of the screening question an* exploring avenues for intervention. To date, the team has interviewed nearly 80 patients who *eported a lack of companionship. Several different options for intervention were presented to the patients; the preliminary results suggest that this population has a great interest in aid services and volunteer opportunities. In the future, similar studies need to be performed
for the other major issues followed by the implementation of these interventions (Poster presented at the Kansas Academy of Family Physicians, 2019).
The Nehru-Fulbright Study
This work has been formative in my young career, and it inspired my current work in India. The main crux of my study is this, “How are SDoH issues addressed at the primary care level in India?” I was interested to see how healthcare workers think about these issues in practi*e, how capacity and workflow encourages or discourages this emphasis, and how financing influenc*s this aim. My main methods of data collection are general observation and informal
interviews. To date, I have visited eleven
clinics; I have visited three public PHC’s and eight private clinics. In order t* summarize the results, I have illustrated a few case studies below.
Case Studies
I wanted to title the first case, “The Minimalist.” This cl*nic is owned and operated *y one individual. He has been practicing for *ver forty years, and to an outsider, his model was truly astounding. This is a small, one-room clinic. The doctor sees about 4-5 patients per hour, and h* charges Rs. 50 per visit. This is an incredible price for the city of Bangalore. In fact, it is the lowest private price I have observed thus far. This physician frequently discusses the SDoH. I have seen him address *ome stress, education
levels, a*d diet patterns. Frankly, I was really encouraged by this practice. My main takeaways from this clinic were the affordability of cutting down on administration and the power of individual good will. To date, the cheapest private clinics I have observed have unanimously been these one-man models. While there are sacrifices in efficiency and community contact, these models certainly remove much of the price barrier to primary care for low- income individuals. In addition to this, I recognize that these physicians have made personal lifestyle sacrifices to provide this kind of care. For one, they have sacrificed salary. Secondly, they have sacrificed time as they have assumed the primary role of caring for their pat*ent population.
The second model is called “The partnership.” This is an urban government PHC. However, it has been contracted out to be run by a private company. In addition to the s*andard government funding, this clinic also receives funds from private entities to bolster its services. This clinic staffs 18 individuals, one of whom is a full-time *octor. The doctor sees 70-80 patients per day. I *ound this fact bewildering. The services here are free. *urprisingly, this building is beautiful and full of amenities. This is largely a result of private funding.
My main takeaways from this clinic are threefold. First, I have started to see that the PHC model is an excellent one. Unfortunately, I have also heard of issues with staffing, medication supply, and bribery within these structures. Secondly, I am
learning about the importance of personal accountability in regards to the SDoH. One key feature of the PHC is the community health workers. In fact, the only way the d*ctor could possibly see so many patients in a day is the assurance that ASHA workers will fo*low-up with patients. This personal contact with a community is amazing, and I believe it is necessary for a primary care clinic to truly invest in social well-being. Finally, I have seen the importance of demographic responsibility. Contrary to all private clinics, a PHC is assigned a given population, called a ward. This is the population for whom the doctor is responsible. Thus, the doctor has a clear target for community health. Because the patients are sorted geographically, the doctor can address structural issues that will cover her entire patient popul*tion.
The third model is called, “The Start-Up.” Broadly, these are the private clinics that consis* of a robust staff of nurses and administration. In this specific case, the physician was just launch*ng her practice. Her staff is eight total. She sees three to four patients p*r hour, and the consultation fee is Rs. 400. My main takeaway from this model is th* business of medicine. I do not believe that this physician has ill-intentions. However, the simple financial demands of operating a clinic make tackling the SDoH very difficult. For one, these clinics often charge the costliest consultation fees. This must be, at least in part, in order to pay the extra staff to run the clinic. These physicians also take on a fair amount of risk to start a practice like this. Moreover, the problem of a
scattered patient population remains. In the end, I cannot imagine that the exis*ence of another primary care clinic is ever bad, but I do worry that such a model may never truly be able to address the roots of health issues.
My last study cas* is titled, “Quality First.” Like the previous model, this is also a private, urban clinic. Two doctors practice in this space, and they have employed a nurse administrator, a lab tech, and a guard for the front. The physicians see eight to ten patients per hour; the consultation fee is Rs. 200 per consultation. Initially, I thought this price seemed on the lower side. During the interview, the physician highlighted that this is actually the most expensive clinic in the area. His explanation is that quality care saves money in the end. Even though his patie*ts are largely low- to middle-income, they will spend the mon*y to see him because they know that it will save them money in the long run. I found this to be a very interesting point. Until now, I had focused mostly on the importance of reaching an entire community, but I had not accounted for the in*reased cost burden of poor care. Even the best physicians cannot offer quality care and address health promotion if bound by enormous time constraints.
Best Practices
I have also been priveleged to visit a few set- ups that I will title best practices in the field. I have visited two similar models, ASHWINI hospital and the Tribal Health Initiative (THIT). To begin, these are bot* clinics that have taken responsibility for a specific,
underserved, geographic community. Without a doubt, the medical care offered at these facilitiesis to be praised. The THI runs a massive *utpatient clinic, seeing nearly 600 patients a week. They also run a 30-bed hospital and provide other services (like dental and diagnostics) as well. Still, what is more impressive is the investment in community health. Many of the staff at ASWHINI hospital are actually from the commmunity (75%). Both hospitals have established *rograms to train community health workers and nurses. Not only does this improve the care of the community, but it also increases the economic stability of the region at large. Moreover, THI has established two oth*r community health initiatives: SOFA and PORGAI. SOFA is an organic farming association. They provide resources and training to local farmers in order to increase the quality of food they produce, and, in turn, in*rease their income. PORGAI is a women’s craft initiative. Wome* from the reg*on work to create clothing and other p*oducts from organic materials grown in the area. This initiative accomplishes several aims: it preserves community practices o* c*atsmanship, it provides financi*l stability, and it prevents migration. In addition to these efforts, these organizations are working on education and political engagement as well. This practice truly is the epitome of community health, and we can only hope *nd pray for more driven individuals to take up such aims.
Concluding Thoughts
In closing, I want to leave you with four points. First, never underestimate the power of an individual. The best models I have observed for really investing in community health is an individual who has sacrificed prestige, money, or comfort to truly take responsibility for the health of a community. Second, if we cannot create motivation, we must, at least, create appeal* While the structure exists for PHC’s to really invest in community health, I have heard that many of the buildings stand empty. One option includes investing in higher salarie* for PHC doctors, investing in the education in the area, or providing adequate support staff. Third, I am becoming ever aware of the impossible balance between quality and quantity. Unfortunately, it will always be difficult to provide quality care to mass populations. One clinic may provide great care to a small few and another may see as many as possible. As we pursue community health, it is important to understand the difficulty of this balance. Finally, I would like to stat* that there is a difference between health and medicine. Medical care is necessary, but I feel like we have o*er-emphasized it as of late. We must remember that healthcare must, first and foremost, be about health. * cannot claim that the healthcare field holds all the answers to a just and equitable society; however, I do think that health*are has a major role to play in accomplishing true community health.
Acknowledgements
The author would like to thank several groups of people for their unique contributions to the work. Dr. Kevin Sykes served as a stateside
mentor to the author, and he contributed to the design and proposal of this project. Dr. Jennifer Woodward and Megan Murray were responsible for much of the work discussed at the University of Kansas. Their inviting the author to participate in the study on social isolation proved to be a formative first step for the current Fulbright project. Dr. RK Prasad serves as the director of research at the Academy of Family Physicians in India. He has worked to *acilitate connections between the author and primary care clinics throughout Bangalore. In addition, he has been a trustworthy gu*de in the data collection and interpretation phases of the project. In addition, Dr. Swathi S B has served as a sounding board and confidante in this work. Her insight into the Indian healthcare system *as g*eatly aided the author in identifying sites and interpreting results. Finally, Dr. Upendra Bhojani and Dr. Dorothy Lall have been generous and wise mentors from the Institute of Public Health in Bangalore. Without their initial interest, this work would not have been possible. Their unique insight and professional expertise helped to shape the project, and they continue to support the work on a regular basis.
-
1. Blue Zones—Live Longer, Better. Blue Zones. https://www.bluezones.com/. Accessed January 23, 2020.↩
-
2. Power 9®. Blue Zones. November 2016. https://www.bluezones.com/2016/11/pow er-9/. Accessed January 23, 2020.↩
-
3. WHO | About social determinants of health. WHO.
-
4. McGinnis JM, Williams-Russo P, Knickman JR. The Case For More Active Policy Attention To Health Promotion. Health Aff (Millwood). 2002;21(2):78-93. doi:10.1377/hlthaff.21.2.78↩
-
5. Booske BC, Athens JK, Kindig DA, Park H, Remington PL. COUNTY HEA*TH RANKINGS WO*KING PAPER. :22.↩
-
6. McKeown T. The Role of Medicine: Dream, Mirage, or Nemesis? Princeton University Press; 1979.↩
-
7. Braveman P, Gottlieb L. The Social Determinants of Health: It’s Time to Consider the Causes of the Causes. Public Health Rep. 2014;129(Suppl 2):19-31.↩
-
8. How Does the U.S. Healthcare System Compare to Other Countr*es? https://www.pgpf.org/blog/2019/07/how- does-the-us-healthcare-system-comp*re- to-other-countries. Accessed January 23, 2020.↩
-
9. Bradley E, Taylor L. The American Health Care Paradox: Why Spending More Is Getting Us Less. Public Affairs; 2013.↩
-
10. How Your Zip Code Could *ffect Your Lifespan | Time. https://time.com/5608268/zip-co*e- health/. Accessed January 23, 2020.↩
-
11. Fair Progress? : Economic Mobility Across Generations Around the World. https://op*nknowledge.worldbank.org/han
-
12. Berman M, Crane R, Seiber E, Munur M. Estimating the cost of a smoking employee. Tob Control. 2014;23(5):428- 433. doi:10.1136/tobaccocontrol-2012- 050888↩
-
13. Obesity and Workers’ Comp Costs. https://www.insurancejournal.com/magazi nes/mag-features/2013/01/14/276698.htm. Accessed January 23, 2020.↩
-
14. Van Nuys K, Globe D, Ng-Mak D, Cheung H, Sullivan J, Goldman D. The association betw*en employee obesity and employer costs: evidence from a panel of U.S. employers. Am J Health Promot AJHP. 2014;28(5):277-285. doi:10.4278/ajhp.120905-QUAN-428↩
-
15. Kowlessar NM, Goetzel RZ, Carls GS, Tabrizi MJ, Guindon A. The Relationship Between 11 Health Risks and Medical and Productivity Costs for a Large Employer. J O*cup Environ Med. 2011;53(5):468– 47*. doi:10.1097/JOM.0b013e31821586b8↩
-
16. Ravussin E, Valencia ME, Esparza J, Bennett PH, Schulz LO. Effects of a Traditional Lifestyle on Obesity in Pima Indians. Diabetes Care. 1994;17(9):1067- 1074. doi:10.2337/diacare.17.9.1067↩
-
17. Natural sleep cycles identified in rural community. ScienceDaily. https://www.sciencedaily.com/releases/20 15/03/150318074513.htm. Accessed January 24, 2020.↩
-
18. Ma Q, Pei G, Jin J. What Makes You Generous? The Influence of Rural and Urban Rearing on Social Discounting in China. PLOS ONE. 2015;10(7):e0133078. doi:10.1371/journal.pone.0133078↩
-
19. Idler E, Blevins J, Kiser M, Hogue C. Religion, a social determinant of mortality? A 10-year follow-up of the Health and Retirement Study. PLOS ONE. 2017;12(12):e0189134. doi:10.1371/journal.pone.0189134↩
-
20. You Asked: Do Religious People Live Longer? Time. https://time.com/5159848/do-religious- people-live-longer/. Accessed January 24, 2020.↩
-
21. Nikkhah H, Nia M, Sadeghi S, Fani M. The Mean Difference of Religiosity between Residents of Rural A*eas and Urban Areas of Mahmoudabad City. Asian Soc Sci. 2015;11. doi:10.5539/ass.v11n2p144↩
-
22. Epidemiology of Social Isol*tion: National Health and Aging Trends Study | The Jou*nals of Gerontology: Series B |
Oxford Academic. https://academic.oup.com/psychsocgeront ology/article/75/1/107/4953727. Accessed January 24, 2020.↩
-
23. Grover. Loneliness: Does it need attention! http://www.jgmh.org/article.asp? issn=2348- 9995;ye*r=2019;volume=6;issue=1;spage =1;epage=3;aulast=Grover. Accessed January 24, 2020.↩
-
24. Social isolation, loneliness in older people pose health risks. https://www.nia.nih.gov/news/social- isolation-loneliness-older-people-pose- health-risks. Accessed January 24, 2020.↩
-
25. RWJF - Qualitative Research Guidelines Project | Informal Interviews | Informal Interviewing. http://www.qualres*org/HomeInfo- 3631.ht*l. Accessed January 22, 2020.↩

Issue: Volume 4, Issue 2 Article
Life-Long Learning Strategies for Famil* Physicians
Dr Devashish Saini (Family Physician and Life-long Learner)
"Education is not something you can finish." - Isaac Asimov
Dr Raghav and Dr Rajni are two close friends who studied together in medical college. After graduating from MBBS, life has taken them on v*ry different paths. But whenever they m*et and share their stories, they realise that they have been facing pretty much the same challenges! And one big mountain they climb on a regular basis is that of life-long learning. Let's see the 3 guidelines and 9 strategies these two doctors have developed to continually hone t*eir skil*s.
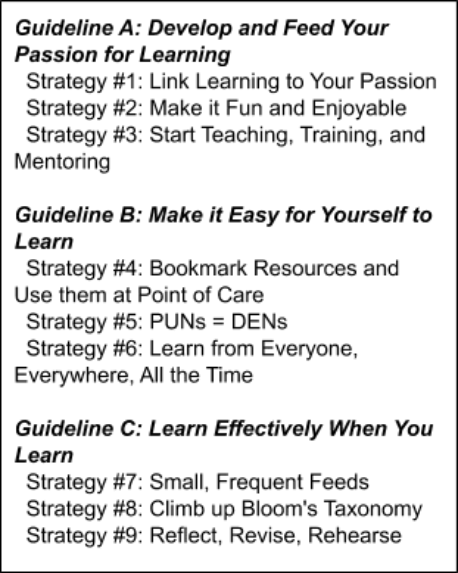
Guideline A: Develop and Feed Yo*r Passion for Learning
Dr Raghav fe*t very demoralised by the low quality of teaching in his medical college, and w*s almost ready to quit medicine by the e*d of his internship, when his uncle invited him to join his established practice as an apprentice.
The way his uncle taught him, as well as learnt himself, was completely grou*d- breaking for Dr Raghav. He developed a new passion for learning and found that he really enjoyed being a physician! These are the three strategies he took away from that experience and he still uses them regularly!
Strategy #1: Link Learning to Your Passion
In the first few weeks of the apprenticeship, Dr Raghav's uncle asked him several questions about his likes, dislikes, and passions, and when he discovered Dr Raghav's passion for cricket, he started using a lot of cricket metaphors to drive home his points.

When Dr Raghav spent half an hour counselling a patient with newly diagnosed hypertension, his uncle praised him for putting in the effort, but also gently suggested to view hypertension management as a test match rather than a T20. The best strategy for a batting partnership in a test match is for the batsmen to *ettle down on the pitch and gradually build the score through ones and twos and the occasional boundaries.
In much the same way, a patient with recent- onset hypertension needs time to come to te*ms with their illness, to bring about the behaviour changes needed to manage their blood pressure, and to develop a lasting relationship with their doctor. It helps if the doctor is cool and relaxed, and happy with the slow and steady progress towards a perfect control of blood pressure through an ever- improving lifestyle!
Dr Raghav told this story to Dr Rajni, who said, "It's funny, a very similar thing worked for me too!" Dr Rajni had a baby just after MBBS, and had joined a distance learning course in maternal and child health. She was finding the course material extremely boring and uninspiring, and was about to drop *ut from the course, when some super-excited relative gifted a set of pastel colours meant for professional painters to their two month- old daugh*er!
Dr Rajni was reminded o* her passion for painting, and started colouring the diagrams in the course material, and then making colourful notes herself using that colour set. That increased her retention of the course material, and she did so well in the exam that she topped her batch!
She has done several courses since then, and the colours have always helped her excel in every course.
Strategy #2: Make it Fun and Enjoyable
Dr Raghav said, "The colour thing sounds fantastic. We had a classmate who used to colour all his books and notes with highlighters of 3 different colours. We used to laugh at him, but looking back now, he used to enjoy his study time much more than any of us did! I'm not an artist, but I can see how colours could make learning more fun."
Dr Rajni said, "Yes, and I found another way to make l*arning interesting. There are tons of videos on YouTube and elsewhere, on each and every topic under the sun! They're made by enthusiastic people whose love for the subject shines through in their teaching, plus they use lots of colourful diagrams, keep making jokes in between, and best of all, we can learn at our own pace!"
Dr Raghav said, "Yes, Khan Acad*my's videos are legendary. I watched this video on the electrical conduction system of the heart* and I've never looked at hearts the same way again! (https://www.khanacademy.org/science/health -and-medicine/circulatory-system/he*rt- depolarization/v/electrical-system-of-the- heart) I also find it interesting to learn from stories. My uncle has lots of patient stories, and when he isn't making te*ri*le cricketing metaphor*, he*s sharing an exotic story about a patient who taught him something or the other!"
Dr Rajni said, "I agree, stories capture our imagination, and help us relate better to the learning material. Also, I find it very enjoyable to learn in a group! All the courses I've attended used to give us group assignments, engage us in group discussions, and the learning groups we formed are still alive to this day. We keep discussing interesting patients, latest articles and guideli*es, and adding our collective experience to the evidence adds a lot of value too!"
On his way back home after this conversation, Dr Raghav is reflecting on the*r discussion, and decides to start doing more learning activities on their batch's WhatsApp group - after all, there should be more to a p*ofessional group *han wishing each other on festivals and birthdays! But he also realises h* enjoys discussing things in person much more than online. He decides to start a Doctors Club in his hometown, where a few FPs can meet regularly and focus on updating
their skills and knowledge. He decides to start by sharing the most fun learning resources he's found and his most engaging patient stories in these groups!
Strategy #3: Start Teaching, Training, and Mentoring
Dr Rajni is also reflecting on their conversation, and remembers that during the courses, she was assigned a few topics to prepare and teach to the whole class, and she can recall them very vividly. When*ver she thinks of learning a new procedure, she can hear her surgery professor's voice in her head, "See one, do one, teach one", and she decides to start t*aching, training, and mentorship of young doctors, and make them as passionate about learning as she is.
In the next few days, she's toying with a few ideas: starting a YouTube channel, painting a colourful medical book, starting online group learning courses, etc. She's unable to travel as she's going through a complicated pregnancy. Then inspiration strikes: She's going to start a series of online video lectures, in which she's creating colourful medical not*s on common topics! Once there are enough of such lectu*es, she can create a course around it, in which she will ask participants to create such
colourful notes themselves, with her support and supervision!
She excitedly shares her idea with Dr Raghav, who says, "I'm going to be your first student, and then I'm going to enrol the whole of our Doctors Club in your cou*se!" Dr Rajni says, "That's great! Give me some ideas for topics you'd like to learn!" Dr Raghav consults his Doctors Club, and they decide they want to learn a vast range of topics, from core clinical skills like confidently reading ECGs and methodically investigating anaemia, to communication skills like breaking bad news and smoking cessation counselling, to practice management topics like managing finances and improving quality of care and services in their clinics. Dr Rajni likes their list: the more variety in the learning topics, higher the fun quotient!
Dr Raghav also decides to utilise every opportunity to educate, teach and mentor everyone around him: his patients and their families, his nurses and other staff, his neighbours and community. He's even started writing for newspapers, going on radio channels, and getting paid health talk assignments. His fun lecture on handwashing has become so popular that he's now fondly known as the Hand Wash Doctor in the whole town!
Guideline B: Make it Easy for Yourself to Learn
As their live* and practices get busier, both Dr Raghav and Dr Rajni realise that it takes a
lot of effort to continually learn and keep abreast of the latest m*dical developments. Th*nkfully, over the years, they have developed techniques and tricks to incorporate the lear*ing process in their daily routine. These are the 3 strategies that have worked for them.
Strategy #4: Bookmark Resources and Use them at Point of Care
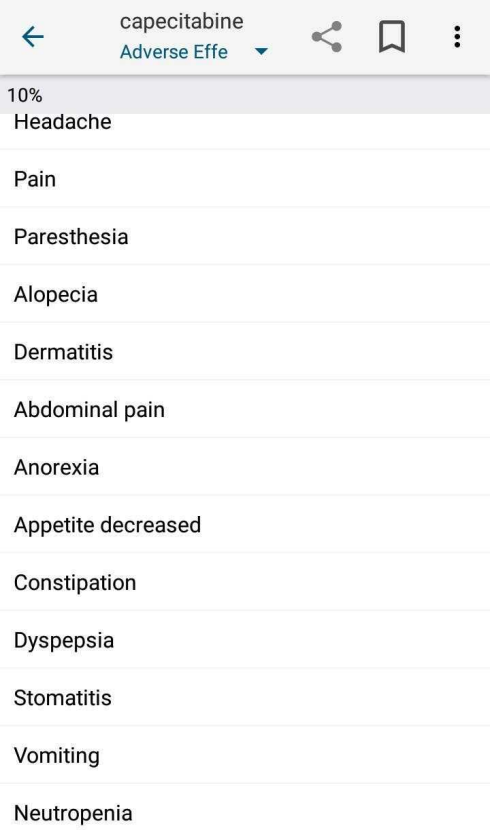
Just the other day, Dr Raghav came across a challenging patient. This was a 67 year old lady he had seen several times before in his clinic. She complained of abd*minal pain, nausea and loose motions for which she was
taking Imodium. The pain was crampy, in lower abdomen, and relieved by pas*ing motions, which were semi-loose 3-4 per day.
She further shared that she was undergoing treatment for breast cancer. She was first diagnosed 6 years back, and got remission with surgery and chemotherapy at that time, but cancer had recurred 5 months back, and had metastasized, for which palliative chemotherapy was started with capecitabine and docetaxel.
Dr Raghav confessed to the patient that he didn't know about these medicines, and opened up Medscape app on his phone. He searched for capecitabine and in the Adverse Effects section he could find all the symptoms that the patient was complaining of. He also glanced at his favourite resource, the Scottish Palliative Care Guid*lines, to see what pain medication would work best for her cramps. (https://www.palliativecareguidelines.scot.nhs .uk/) He gently explained what all he had found to the patient and her husband, and prescribed medicines for s*mptomatic relief, fluids, and probiotics. He suggested them to contact their oncologist in case these treatments didn't give her relief. The family thanked him for his extra effort, and went away satisfied.
Dr Raghav mentally thanked the creators of Medscape, his favourite point-of-care resource, which had greatly increased the range of conditions he could confidently manage. He decided to share his experience of Medscape in the next Doctors Club
meeting, and ask other members what resources they've bookmarked on their phone or computer for looking up during consultation itself. He also resolved to get an UpToDate subscription soon, maybe as a birthday present for himself!
Strategy #5: PUNs = DENs
Even after doing everything he did for his patient, Dr Raghav had a nagging feeling that there could be more he could have done. Before calling in the next patient, he fired up the Notes app on his phone, opened the Note
titled "PUNs" and added: "Management of chemotherapy-associated diarrhoea" at the top.
*e had started keeping track of such points after attending a workshop in * conference where they taught the simple yet powerful concept of PUNs = DENs. Stated fully, Patients' Unmet Needs are equal to Doctor's Educational Needs. In other words, the doctor needs to recognise where they're not able to meet the needs of their patients, and gear up to gather the skills and knowledge needed to fulfill those needs.
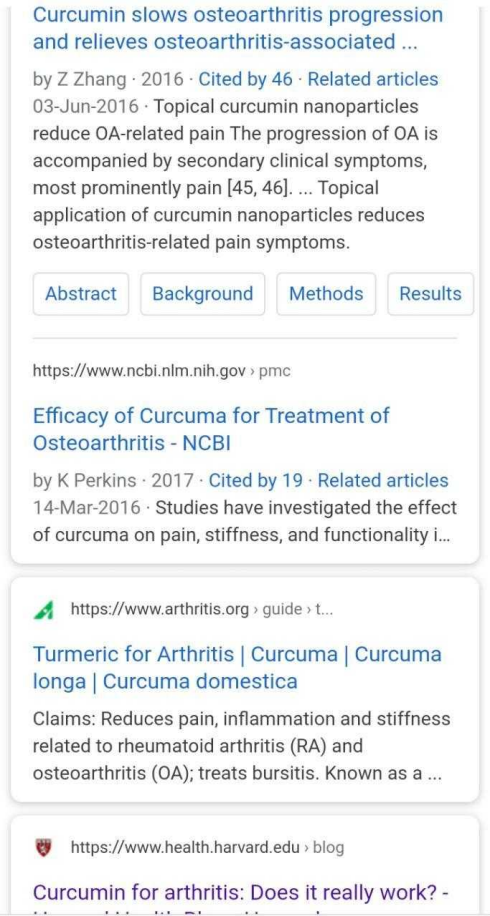
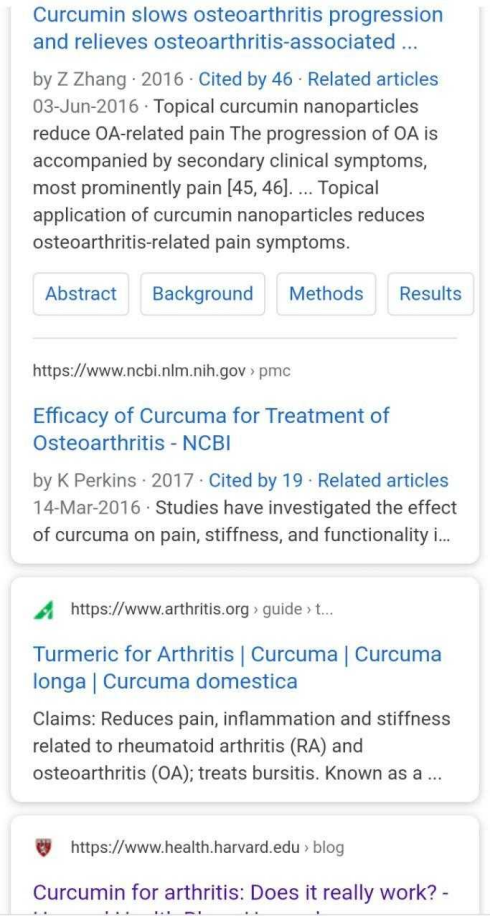
While travelling by auto from clinic to home that night, Dr Raghav opens up the list of PUNs again on his phone, and reviews them. He finds that a common PUN in the last week in his clinic relates to the use of supplements in patients with osteoarthritis. He decides to educate himself about it.
From his previous learning experiences, he knows that books are unlikely to be helpful, as they would not incorporate the latest research of last few years. He searches on his trusted Medscape app and finds that "glucosamine-chondroitin and glucosamine or chondroitin sulfate alone show medium- term benefits with no long-term benefits for pai* or function."
There's no mention of curcumin, which some of *is patients hav* been prescribed by other doctors. He tries a Google search, and it seems there's a lot of hype about curcumin for osteoarthritis. To dig deeper he opens and reads an article on this topic on the Harvard
Health Blog. (https://www.health.harvard.edu/blog/curcum in-for-arthritis-does-it-really-work- 2019111218290) After reading the article, it's clear t*at all the hype is just based on one small study. He decides to wait for more studies before he starts prescribing it himself, and if patients ask him about it, he can share with them what *e's found today, in simple terms they can understand, and let them make up their minds whether they want to stop taking it or to continue.
Strategy #6: Learn from Everyone, Everywhere, All the Time

Dr Raghav still has a few minutes to reach home. He remembers the spirited discussion t*ey had on the movie Drishyam in the last Doctors Club meetup. They discussed how doctors can use the power of positive imagery to challenge and change the negative narratives people have in their minds, about themselves, their family and their disease.
Dr Vani, a new member of the *lub, shared how she uses this *echnique to counsel parents who complain in front of their children, "He/she doesn't eat any fruits or vegetables!" Dr Vani asks the child, "Which fruit do you like? I love apples, do you like apples too?" Typically the child says the
name of one or two fruits and vegetables that they like, Dr Vani congratulates him/her on that, and continues to build on the positivity, finally suggesting parents to use positive imagery like enjoying fruits and vegetables in front of children to get them to eat healthier! Dr Raghav also tried this technique with his patients, and it seemed to work!
In the coming meetu*, he's looking forward to talking about this book he read last month "When Breath Becomes Air". The insights from this autobiography of a dying neurosurgeon will surely help the doctors change the way they take care of end-of-life patients, specifically, to help them find meaning in the last few days of their life. In fact, in recognition of the multiple roles a Family Physician plays, the Club has started devoting the first 15-20 minutes of their meetup to discuss an art piece, and how they can use the lessons to change the way they practice the Art of Medicine. This includes paintings, sculptures, movies, short films, Ted Talks, poems, hymns, novels, etc etc. They even discussed learnings from a Saas Bahu serial once!

Wi*h that thought, Dr Raghav looks outside the auto and *ealises that learnings are
everywhere around us! We can learn customer service from our friendly neighbourhood chai wallah, discipline from the milkman, playfulness from young children, IT skills from the nerdy cousin, social media strategies from our competition, and how to brave adverse environment from the plants and trees growing in our yard!
Guideline C: Learn Effectively When You Learn
It seems to Dr Rajni that the more she learns and teaches, the more she realises how much more there is to the teaching and mento*ship *rocess. She's very much appre*iative of all the teachers in her life who not only made the learning fun but also long-l*sting. Now that she's a teacher herself, she makes sure to incorporate these three strategies below to enhance the effectiveness of the learning process.
Strategy *7: Small Frequent Feeds
In the initial days of *eaching, she used to frequently encounter glazed eyes within 10 minutes of her starting to speak on a particular topic. She discussed this with Dr Raghav, who said, "Here comes my uncle's cricket metaphor: There's a reason why an over is only 6 balls, and the bowlers and batsmen have to change at the end of the over. Efficiency dec*eases if we overload our senses." Dr Rajni said, "So you're saying I might be giving them too much information?" Dr Raghav said, "Could be, after all most of us can only hold and process maximum 3 concepts in our brain at one time!"
Dr Rajni reflected and agreed that in her zeal of teaching, she was overloading her slides with l*arning material. She started reducing the content on each slide, breaking the concepts into smaller chunks, and v*ila! her students were much more attentive and engaged since then! She uses the same technique on herself now, reading up a topic in b*ts and pieces, taking time to digest and reflect and only then reading further.
Strategy #8: Climb Up *loom's Taxonomy

Dr Rajni has another technique to prevent students turning to their mobile phones while in her class. Before each session, she reflects on the background of her learners, where they're practicing and how they're going to use the learnings from her session. She then defines 1-3 specific learning objectives (SLOs) for her session, and they help her to make the material super-focus*d, and to keep the attention of the class throughout the session!
She recently came across a very interesting paradigm called Bloom's Taxonomy and she's started using it to create these SLOs. If most of her students have crossed the "Remember" and "Understand" levels, then she creates the objective around "Applying" the concepts t*
solve real-life problems. E.g. applying an algorithm to rationally investigate anemia in patients. Once this is defined, it's very clear that she doesn't need to focus on explaining the algorithm itself* rather on taking the participants through various patient scenarios and applying the algorithm to rationally investigate each patient.
This same technique she uses to better define her DENs every week, and choose the learning strategy that best fits that need. If she needs to remember something, she uses mnemonics, flash cards, vivid imagery and of course, her favourite tool, painting with colours, to enhance the chances of the material sticking in her mind.
And s*e strives to climb ever higher on the taxonomy ladder!
Strategy #9: Reflect, Revise, Rehear*e
"This last strategy can't be repeated enough!" Dr Rajni chuckles to herself, and vows to never subject her students to this terrible PJ. She does however recall several lectures and courses that repeated their key take home message again and again in various different ways. She specifically remembers an engaging lectur* she attended on recent advances in diabetes, and the faculty kept repeating, "Be obsessed about blood pres*ure!", after every 3 slides, driving home the point that strict control of blood pressure is now conside*ed much more important for the long term health of a diabetic than strict control of their blood sugar.
That lecture changed her practice - she and her clinic staff now regularly measure and strictly mana*e her diabetic patients' blood pressure. And it also changed her teaching. She keeps reiterating the key message throughout the session - in much the same way fans keep asking the score during a cricket match!
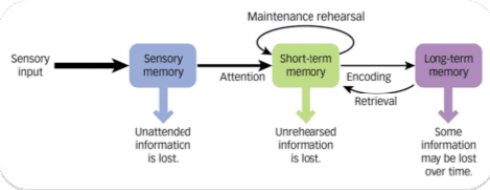
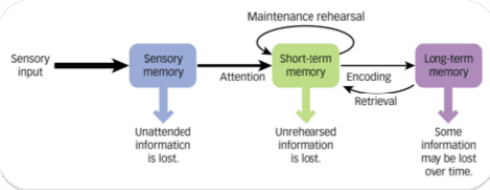
She also encourages her mentees and students to reflect on the day's learnings, and think about how they'll change their practice in the future, before finishing the day's work. And she follows the same practice herself, spending 10 minutes every night reflecting and revising the day's learnings, after putting her kids to sleep. Any memory that's revised within 24 hours has a much higher chance of getting stored in the long-term memory.
Endgame
If you've rea* through this whole article and reached here, I salute you! Can I keep your interest for another two minutes so that we can cement the learnings from this article?
Here's a tr*asure hunt: Out of the nine strategies presented in the article, which strategies have been followed in this article, and which have not? You can keep your answer to yourself, or you can send your answer to me, along with any feedback about this art*cle or even general comments on learning strategies.
Email: devashish@rossclinics.com
WhatsApp: +91-999050*859

Issue: Volume 4, Issue 2 Article
Life-Long Learning Strategies for Family Physicians
Dr Devashish Saini (Family Physician and Life-long Learner)
"Education is not something you can finish." - Isaac Asimov
Dr Raghav and Dr Rajni are two close friends who studied together in medical college. After graduating fr*m MBBS, life has taken them on very different paths. But whenever they meet and share their stories, they realise that they have been facing pretty much the same challenges! And one big mountain they climb on a regular basis is that of life-long learning. Let's see the 3 guidelines and 9 strategies these two doctors have developed to continually hone their skills.
Guideline A: Develop and Fee* Your Passion for Learning
Dr Raghav felt very demoralised by the low quality of teaching in his medical college, an* was almost ready to quit medicine by the end of his internship* when his uncle invited him t* join his established practice as an apprentice.
The way his uncle taught him, as well as learnt himself, was completely ground- breaking for Dr Raghav. He developed a new passion for learning and found that he really enjoyed being a physician! These are the three strategies he took away from that experience and he still uses them regularly!
Strategy #1: Link Learning to Your Passion
In the first few weeks of the apprenticeship, Dr Raghav's uncle asked him several questions about his likes, dislikes, and passions, and when he discovered Dr Raghav's passion for cricket, he started using a lot of cricket metaphors to drive home his points.

When Dr Raghav spe*t half an hour counselling a patient with newly diagnosed hypertension, his uncle praised him for putting in the effort, but also gently suggested to view hypertension management as a test match rather than a T20. The best strategy for a batting part*ership in a test match is for the batsmen to settle down on the pitch and gradually build the score through ones and twos and the occasional boundaries.
In much the same way, a patient with recent- onset hypertension needs time to come to terms with their illness, to bring about the behaviour changes needed to manage their blood pressure, and to develop a lasting relationship with their doctor. It hel*s if the doctor is cool and relaxed, and happy with the slow and steady progress towards a perfect control of blood pressure through an ever- im*roving lifestyle!
Dr Raghav told this story to Dr Rajni, who sa*d, "It's funny, a very similar thing worked for me too!" *r Rajni had a baby just after MBBS, and had joined a distance learning course in maternal and child health. She was finding the course *aterial extremely boring and uninspiring, and was about to drop out from the course, when some super-excited relative gifted a set of pastel colours meant for professional painters to thei* two month- old daughter!
Dr Rajni was reminded of her passion for painting, and started colou*ing the diagrams in the course material, and then making colourful notes herself using that colour set. That increased her retention of the course material, and she did so well in the exam that she topped her batch!
She has done several courses since then, and the colours have always helped her excel in every course.
Strategy #2: Make it Fun and Enjoyable
Dr Raghav said, "The colour thing sounds fantastic. We had a classmate who used to colour all his books and notes with highlighters of 3 different colours. We used to laugh at him, but looking back now, he used to enjoy his study time much more than any of us did! I'm not an artist, but I can see how colours could make learning more fun."
Dr Rajni said, "Yes, and I found another way to make learning interesting. There are tons of videos on YouTube and elsewhere, on each and every topic under the sun! They're made by enthusiastic people w*ose love for the subject shines through in their teaching, plus they use lots of c*lourful diagrams, keep making jokes in between, and best of all, we can learn at our own pace!"
Dr Raghav said, "Yes, Khan Academy's videos are legendary. I watched this video *n the electrical conduction system of the heart, and I've never looked at hearts the same way again! (https://www.khanacademy.org/science/health -and-medicine/circulatory-sy*tem/heart- depolarizatio*/v/electrical-system-of-the- heart) I also find it interesting to learn from stories. My uncle has lots of patient stories, and when he isn't making terrible c*icketing metaphors, he's sharing an exotic story about a patient who taught him something or the other!"
Dr Rajni said, "I agree, stories capture our imagination, and help us relate better to the learning material. Also, I find it very enjoyable to *earn in a group! All the courses I've attended used to give us group assignments, engage us in group discussions, and the learning groups we form*d are still alive to this day* We keep discussing interesting patients, latest articles and guidelines, and adding our collective experience to the evidence adds a lot of value too!"
On his way back home after this conversation, Dr Raghav is reflecting on their discussion, and decides to start doing more learning activities on their batch's WhatsApp group - after all, there should be more to a professional group than wishing each other on festivals and birthdays! But he also realises he enjoys discussing things in person much more than online. He decides to start a Doctors Club in his hometown, where a few FPs can meet regularly and focus on updating
their skills and knowledge. He decides to start by sharing the most fun learning resources he's found and his most engaging patient stories in these groups!
Strategy #3: Start Teaching, Training, and Mentoring
Dr Rajni is also reflecting o* their conversation, and remembers that during the courses, she was assigned a few topics to prepare and teach to the whole class, and she can recall them very vividly. Whenever she thinks of learning a new procedure, she can hear her surgery professor's voice in her head, "See one, do one, teach one", and she decides to start teaching, training, and mentorship of young doctors, and make them as passionate about learning as she is.

In the next few days, she's toying with a few ideas: starting a YouTube channel, painting a colourful medical book, starting online group learning courses, etc. She's unable to travel as she's going through a complicated pregnancy. Then inspiration strikes* She's going to start a series of online video lectures, in which she's creating colourful medical notes on common topics! Once there are enough of such lectures, she can create a course around it, in which she will ask participants t* create such
colourful notes themselves, with her support and supervision!
She excitedly shares her idea with Dr Raghav, who says, "I'm going to be your first student, and then I'm going to enrol the whole of our Doctors Club in your course!" Dr Rajni says, "That's great! Give me some ideas for topics you'd like to learn!" Dr Ra*hav consults his Doctors Club, and they de*ide they want to learn * vast range of topics, from core clinical skills like confidently reading ECGs and methodically investigating *nae*ia, to communication skill* like breaking bad news and smoking cessation counselling, to practice management topics like managing finances and improving quality of care and services in their clinics. Dr Rajni likes their list: the more variety in the learning topics, higher the fun quotient!
Dr Raghav also decides to utilise every opportunity to educate, teach and mentor everyone around him: his patients and their families, his nurses and other staff, his neighbours and community. He's even started writing for newspapers, going *n radio channels, and getting paid health talk assignments. His fun lecture on handwashing has become so popular that he's now fondly known as the Hand Wash Doctor in the who*e town!
Guideline B: Make it Easy for Yourself to Learn
As their lives and practices get bu*ier, both Dr Raghav and Dr Rajni realise that it takes a
lot of effort to continually lea*n and keep abreast of the latest medical developments. Thankfully, over the years, the* have developed techniques and tricks to incorporate the learning process in their daily routine. These are the 3 strategies that have worked for them.
Stra*egy #4: Boo*mark Resources and Use them at Point of Care
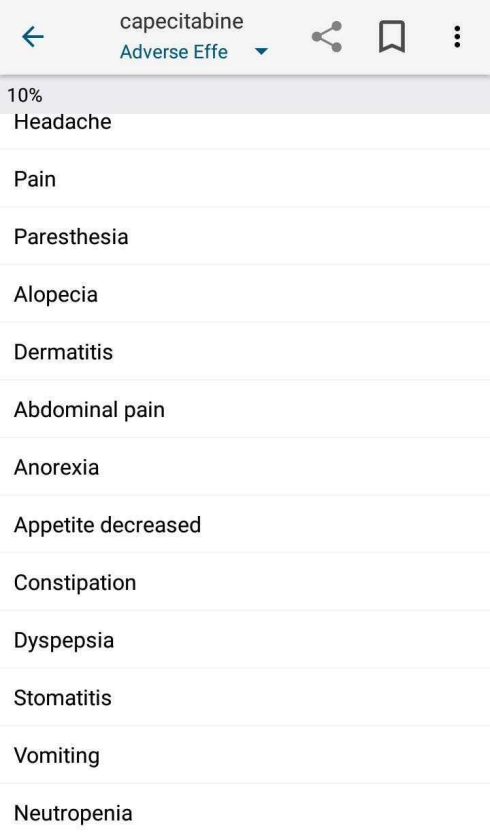
Just the other day, Dr Raghav came across a challenging patient. This was a 67 year old lady he had seen several times before in his cl*nic. She complained of abdominal pain, nausea and loose motions for which she was
taking Imodium. The pain was crampy, in lower abdomen, and relieved by passing motions, which were semi-loose 3-4 per day.
She further shared that she was undergoing *reatment for breast cancer. She was first diagnosed 6 years back, and got remission with surgery and chemotherapy at that time, but cancer had recurred 5 months back, and had metastasized, for which palliative chemotherapy was started with capecitabine and docetaxel.
Dr Raghav confessed to the patient that he didn't know about these medicines, and opened up Medscape app on his phone. He searched for capecitabine and in the Adverse Effects section he could find all the symptoms that the patient was complaining of. He also glanced at his favourite resource, the Scottish Palliative Care Guidelines, to see *hat pain medication would work best for her cramps. (https://www.palliativecareguidelines.scot.nhs .uk/) He gently explained what all he had found to the patient and her husband, and prescribed medic*nes for symptomatic relief, fluids, and probiotics. He suggested them to contact their oncologist in case these treatments didn't give her relief. The family thanked him for his extra effort, and went away satisfied.
Dr Raghav mentally thanked the creators of Medscape, his favourite point-of-care resour*e, which had greatly increased the range of conditions he could confidently manage. He decided to share his experience of Medscape in the next Doctors Club
meeting, and as* other members what resources they've bookmarked on their phone or computer for looking up during consultation itself. He also resolved to get an UpToDate subscription soon, maybe as a birthday pres*nt for himself!
Strategy #5: P*Ns = DENs
Even after doing everyt*ing he did for his patient, Dr Raghav had a nagging feeling that there could be more he could have done. Before calling in the ne*t patient, he fired up the Notes app on his phone, opened the Note
titled "PUNs" and added: "Management of chemotherapy-associated diarrhoea" at the top.
He had started keeping track of such points after attending a workshop in a conference where they taught the simple yet powerful concept of PUNs = DENs. Stated fully, Patients' Unmet Needs are equal to Doctor's Educational Needs. In other words, the doctor needs to recognise where they're not able to meet the needs of their patients, and gear up to gather the skills and knowled*e needed to fulfill those needs.
While travelling by auto from clinic to home that night, Dr Raghav opens up the list of PUNs again on his phone, and reviews them. He finds that a common PUN in the last week in his clinic relates to the use of supplements in patients with osteoarthritis. He decides to edu*ate himself about it.
From his previous learning experiences, he knows that books are unlikely to be helpful, as they would not incorporate the latest research of las* few years. He searches on his trusted Medscape app and finds that "glu*osamine-chondroitin and glucosamine or chondroitin sulfate alone show medium- term benefits with no long-term benefits for pain or function."
There's no mention of curcumin, which some of his patients have been prescrib*d by other doctors. He tries a Google search, and it seems there's a lo* of hype *bout curcumin for osteoarthritis. To dig deeper he opens and reads an article on this topic on the Harvard
Health Blog. (https://www.health.harvard.edu/blog/curcum in-for-arthritis-does-it-really-work- 2019111218290) After reading the article, it's clear that all the hype is just based on one small study. He decides to wait for more studies before he starts prescribing it himself, and if patients ask *im abou* it, he *an share with them w*at he's found today, in simple terms they can *nderstand, and let them make up their minds whether they want to stop taking it or to continue.
Strategy #6: Learn from Everyone, Everywhere, All the Time

Dr Raghav still has a few minutes to reach home. He remembers the spirited discussion they had on the movie Drishyam in the last Doctors Club meetup. They d*scussed how doctors can use the power of positive imagery to challenge and change the ne*ative narratives people have in their m*nds, about themselves, their family and their disease.
Dr Vani, a new member of t*e club, shared how she uses this technique to counsel parents who complain in front of their children, "He/she doesn't e*t any fruits or vegetables!" Dr Vani a*ks the child, "Which fruit do you like? I love apples, do you like apples too?" Typically the child says the
name of one or two fruits and vegetables that they like, Dr Vani congratulates him/her on that, and continues to build on the positivity, finally suggesting parents to use positive imagery like enjoying fruits and vegetables in front of children to get them to eat *ealthier! Dr Raghav also tried this technique with his patients, and it seemed to w*rk!
In the coming meetup, he's looking forward to talking about this book he read last month "When Breath Becomes Air". The insights from this autobiography of a dyin* neurosurgeon will surely help the doctors change the way they take care of end-of-*ife patients, specifically* to help them find meaning in the last few days of their life. In fact, in recognition of the multiple roles a Family Physician plays, the Club has started devoting the first 15-20 minutes of their meetup to discuss an art piece, and *ow they can use the lessons to change the way they practice the Art of Medicine. This includes paintings, sculptures, movies, short films, Ted Talks, poems, hymns, novels, etc etc. They even discussed learnings from a Saas Bahu seria* once!

With that thought, Dr Raghav looks outside the auto and realises t*at learnings are
e*erywhere around us! We can learn customer service from our friendly neighbourhood chai wallah, discipline from the milkman, playfulness from young children, IT skills from the nerdy cous*n, social media strategies from our competition, and how to *rave adverse environment from the plants and trees growing in our yard!
Guideline C: Learn Effectively When You Learn
It seems to Dr Rajni that the more she learns and teaches, the more she realises how much more there is to the teaching and mentorship process. She's very much appreciative of all the teachers in her life who not only made the learning fun but also long-lasting. Now that she's a teacher h*rself, she makes sure to incorporate these three strategie* below to enhance the effectiveness of the learning process.
Strategy #7: Small Frequent Feeds
In the initial days of teaching, she used to frequently encounter glazed eyes within 10 minutes of her starting to speak on a particular topic. She discussed this with Dr Raghav, who said, "Here comes my uncle's cricket metaphor: There's a reason why an over is only 6 balls, and the bowlers and batsmen have to change at the end of the over. Efficiency decreases if we overload our senses." Dr Rajni said, "So you're saying I might be giving them too much information?" Dr Raghav said, "Could be, after all most of us can only hold and process maximum 3 concepts in our brain at one time!"
Dr Rajni reflected and agreed that in her zeal of teaching, she was overloading her slides with learning material. She started reducing the content o* each slide, breaking the concepts into smaller chunks, and voila! her students were much more attentive and engaged since then! She uses the same technique on herself now, reading up a topic in bits and pieces, taking time to digest and reflect and only then reading further.
Strategy #8: Climb Up Bloom's Taxonomy
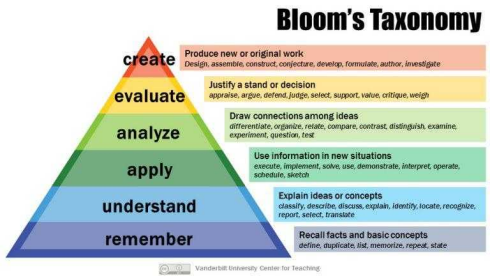
Dr Rajni has another technique to prevent students turning to their mobile phones while in her class. Before each session, she reflects on the background of her learners, where they're practicing and how they're going to use the learnings from her session. She then defines 1-3 specific learning ob*ectives (SLOs) for her session, and they help her to make the material super-focused, and to keep the attention of the class throughout the session!
She recentl* came across a very interesting paradigm called Bloom's Taxonomy and she's started using it to create these SLOs. If most of her students have crossed the "Remember" and "Understand" levels, then she creates the objective around "Applying" the concepts to
solve real-life problems. E.g. applying an algorithm to rationally investigate an*mia in patients. Once this is defined, it's very clear t*at she doesn't need to focus on explaining the algorithm itself, rather on taking the participants through various patient scenarios and applying the algorithm to rationally investigate each patient.
This same technique she uses to better define her DENs every week, and choose the le*rning strategy that best fits that need. If she needs to remember somethin*, she uses mnemonics, flash cards, vivid imagery and of course, her favourite tool, painting w*th colours, to enhance the chances of the material sticking in her mind.
And she strives to climb ever higher on the taxonomy ladder!
Strategy #9: Reflect, Revise, Rehearse
"This last strategy can't be repeated enough!" Dr Rajni c*uckles to herself, and vows to never subject her students to this terrible PJ. She does however recall several lectures and courses that repeated their key take home message again and again in various dif*erent ways. She specifically remembers an engaging lecture she attended on recent advances in diabetes, and the faculty kept repeating, "Be obsessed about blood pressure!", after every 3 slides, driving home the point that strict control of blood pressure is now considered much more im*ortant for the long term health of a diabetic than strict control of their blood sugar.
That lecture changed her practice - she and her clinic st*f* now regularly measure and strictly manage *er diabetic patients' blood pressure. And it also changed her teaching. She keeps reiterating the key message throughout the session - in much the same way fans keep asking the score during a cricket match!
She also encourages her mentees and students to r*flect on the day's learnings, and think about how they'll change their practice in the future, before finishing the day's work. And she follows the same *ractice herself, spending 10 minutes every night reflecting and revising the day's learnings, after putting her kids to sleep. Any memory that's revised within 24 hours has a much higher chance of getting stored in the long-term memory.

Endgame
If you've read through this whole article and reached here, I s*lute you! Can I keep your interest for another two minutes so that we can cement the learnings from this article?
Here's a treasure hunt: Out of the nine strategies presented in the article, which strategies have been followed in this article, and which have not? You can keep your answer to yourself, or you can send your answer to me, along with any feedback about this article or even general comments on learning strategies.
Email: devashish@rossclinics.*om
WhatsApp: +91-9990505859

Issue: Volume 4, Issue 2 Practice Experience
Dilemmas of a GP
Dr Swapna Bhaskar (President - AFPI Karnataka; HOD - Family medicine, St. Philomena's Hospital)
On a usual busy morning in my hospital OP, a gentleman in his 60s walked in with his young daughter who, unlike him, was well- dressed and spoke fluent English.
With one look at his puffy erythematous face, the diagnosis of “chronic ethanol abuse” flashed in my mind.
He started narrating his story. He had been sent by the pastor of the local church for free treatment here. Ours is a charitable, missionary hospital wh*re we get many self- proclaimed charismatic men and women apart from actual members of diff*rent religious congregations.
He had a swelling in the submental region for 3 months and another slowly growing swelling in the neck causing mechanical symptoms. This needed a resection and biopsy at the earliest. He was found to have high BP and blood sugar on routine check up along with weight loss, breathlessness on
exertion, and *igns of p*ripheral neuropathy and fluid overload. A Pandora’s box was being slowly opened.
He was diagnosed with hypothyroidism 9 years before and was on a 50 mcg replacement dose. But not a single thyroid pro*ile was done in those years. “But I take the tab regularly and I have no symptoms of thyroid” he answered, looking irritated when I asked him about his apath*! Added to it was the financial difficulty, he said, and that was when he approached the church where he belonged. The big hearted pastor had agreed to sponsor the treatment he needed.
He proceeded. He had been smoking at least a pack of bidis or cigarettes a day since he was 18 years of age! “It just costs about 10-20 rupees per day”, the justification came promptly from his “English speaking daughter”.
And then came the piece of history t* confirm my spot diagnosis - 2 quarters of hot drinks per day for more than 35 years now. Could I be wrong here? No way!
I began my usual advice about how he needed to get his sugar and blood pressure under control, quit smoking and alcohol consumption, and get all his investigations done thoroughly. To my boring lecture, he replied that he had no finan*ial support for investigations and had to manage with what the pastor gave, yet he needed a solution for his symptoms and fitness for surgery without compromising on his habits!
The doctor in me is in a big dilemma:
-
 How did he obtain finances for all his fancy habits till now?
How did he obtain finances for all his fancy habits till now? -
 How did the pastor not reason before giving him financial support that he is a smoker and alcoholic? * Is that a routine which can be sidelined as normal?
How did the pastor not reason before giving him financial support that he is a smoker and alcoholic? * Is that a routine which can be sidelined as normal? -
 His family supports his habits very well knowing the ills of it – “he needs to be mentally happy at this age” according to them.
His family supports his habits very well knowing the ills of it – “he needs to be mentally happy at this age” according to them. -
 How can we doctors deal with such “impracti*al jokers” as I call them?
How can we doctors deal with such “impracti*al jokers” as I call them?
I am sure many of my friends here will relate to this an* hence penned my thoughts. Aren’t such patient* real social/emotional challenges to us practitioners? I am still looking for solutions.
I haven’t seen the patient in follow-up – he probably found me an “impractical joker”!

Issue: Volume 4, Issue 2 Practice Experie*ce
Food for thought
Dr Roshni Jhan Ganguly (Family Physician)
Here *s a food for thought - Is our commitment to our community putting our families at home at avoidable *isk?
There are many tough questions.
How does one triage patients? How does one keep themselves, their staff and their family safe? Should we shut down clinics? Do I see only patients who have an emergency? When I do so, am I safe? Should I rather do online consultations for them and see only my regula* patients in-person? In the latter case, how do I ensure social distancing and protect the community?
The million dollar question - Am I trying to cure people or am I, inadvertently, spreading the disease in these dismal times?
As health workers we do need to be cognizant of the risks we fa*e, but where do we draw the line between what is an acceptable risk and what is not? We are the frontliners in the health system, the first point o* contact for
our patients. Is our health system prepared to support us and help patients with COVID-19?
It is time we introspect and make changes in the routines of our clinics to keep ourselves safe? There would be the question of affordability. Can we, as family physicians, afford the cost of a separate uniform for clinics, PPEs for ourselves and our staff, and disinfection of our clinics everyday? Can we have housekeeping staff to clean surfaces and door knobs after each patient? How do we sustain then? The government would have to provide support to us should we function this way.
Let's discuss viable options. One that I thought of and wrote for all my patients is this:
📢 In these difficult times of COVID- 19 infection, we pray for your safety and good health wherever you are
Staying at home🏡 and maintaining social distancing is the key to stop the spread of the Novel Corona Virus🦠 .
⚡ You are at risk, but your consultant doctor is at an equal and perhaps more p*rpetual risk⚡.
If you have symptoms of fever🤒 , cough*��� , cold🤧 or breathing difficulty🤢 and if you have a recent history of travel✈ or contact, Please consult the doctor online🖥 using Google hangout.
Hope this initiative of online video consultation helps all. 📱📲Please spread *he message and help one another.
Do you feel it is justified?
Online consultations could be the silver lining of the dark clouds that these challenging times are.

Issue: Volume 4, Issue 2 Opinion
Healthcare Delivery Sy*tem in India – My Reflections
Dr Siddharth V H (GP and Family Physician)
Today I am paranoid, scared, and terrified to go to a hospital myself seeing the attitude of some doctors, who have no concern fo* the patients. I, as a common man, worry about where to take my children in case of a medical problem. My rights as a citizen of India to get a decent *edical care seem to be under siege.
Should I always b* running around for a second opinion? How should I trust my doctor? Of course medicine is not an exact science and there a*e 4-5 different ways of treatment for the same ailment. But whom to trust?
I am not against doctors making money, but the “corporate culture” of making money illicitly in the name of healthcare and driving society into grief stricken poverty is what I oppose. One can deal with poverty and still be happy. But they would be devastated when pushed into poverty and grief through daylight robbery by the people in whose hands they entrust the life of their loved ones.
All doctors are not bad, but there are some b*ack sheeps who dance to the tunes of their corporate bosses, who are bringing a bad name to the whole of Indian doctors.
There needs to be a che*k on the operation of these corporate hospitals. They a*e spending crores of rupees on equipment and feeding patients to these in the name of quality healthcare. The Government has given licenses to them to serve the c*mmunity and not to loot it.
Government should impose that a percentage of their investment is spent on maintaining a universal patient data system and let government hospital doctors be given extra duty of monitoring the treatment if a patient calls a helpline and complains about malpractice. All the history of the patient and the treatment giv*n should be chronologically entered into the system, so that it is easily accessible to patients and other doctors. This would make them more transparent and the
common man will have trust and faith in their doctors.
Already the *octor is reduced to a salespers*n selling his services and has *ost the image of a well wisher of the co*munity. This has to change and this change can only be brought by proper steps taken by the Government to bring about transparency in the system. The government doesn’t have to build hospitals and compete with private hospitals, but bring reforms that would plug all the loopholes that allow malpractice thus turning these slaughter houses into temples where people are happy to go and willingly pay any amount of cost incurred.
Yes, the Government tried to bring some reforms recently by tabling the KPME Amendment act, which was fiercely opposed by the medical fraternity. That bill tried to impose sanctions on money-making policies of these hospitals by bringing price caps on consultations and procedures. Reforms are necessary not to target the earning of the doctor/hospitals but the ethics *f principles followed.
A doctor is an artist. There are good artists and there are not so good artists. The* make money according to their talent and the quality of service the hospital pro*ides. But I am talking about the con artists in the medical fraternity who are not bothered about the community and are giving shoddy, unethical treatment to the public in the name of healthcare and looting them. These con artists need to be eliminated or put in check.
Reforms are needed to protect the good artists and deal with an iron hand with the con artist*. The common man cannot fight them alone, the Government has to step in and set up a transparent system of maintaining a universal health record system, linked to Aadhaar, which can be accessible anywhere. All the treatment g*ven in the hospitals should be uploaded here so that it becomes easier for the patient to get a second opinion and for the court, in cases of negligence, to provide quick relief to the victim instead of him doing all the circus himself to get justice.
The government should at least provide this, if they are not pr*viding good g*vernment hospitals. If this facility is *vailable then, it will put indirect pressure on all the hospitals to provide the right and cost effective care to the patients and will treat them well, b*cause they have to retain them to make money and be in business.
I want to feel safe entrusting the life of my loved ones in the hands of doctors. Money is not the question here. Getting quality health care, *nsuring the well being of the patients by following ethical principles of medical care viz, -- 1) Principle of respect for autonomy, 2) Principle of nonmaleficen*e, 3) Principle of beneficence, and 4) Principle *f justice.
This is the need of the hour, and not getting financially and emotionally drained by visiting thes* hospitals.

Issue: Volume 4, Issue 2
Ethical challenges of digital health technologies: Aadhaar, India
Vijayaprasad Gopichandran (Employees State Insurance Corporation Medical College and Post Graduate Institute of Medical Sciences and Research, Chennai, India)
Parasuraman Ganeshkumar (Indian Council of Medical Research, National Institute of Epidemiology, Chennai, India)
Sambit Dash (Department of Biochemistry, Melaka-Manipal Medical College, Manipal Academy of Higher Educ*tion, Karnataka, India)
Aarthy Ramasamy (Madras Diabetes Research Foundation, No. 4, Conran Smith Road, Gopalapuram, Chennai, 600086, India)
This article was originally published in Bulletin of the World Health Organization under "Lessons from the Field" under a Creative Commons Attribution 3.0 IGO licence (CC BY 3.0 IG0) and is being republished here. The original can be accessed online here.
Introduction
Low- and middle-income countries have experienced a rapid and massive influx of digital and mobile technologies and their *pplications. This information and communication revolution has brought great
benefits for the practice of pu*lic health in these countries. Several studies have shown evidence of effective digital applications in health including electronic health records, digital epidemiology and mobile health
applications. With these massive stri*es in
digital health, important ethical issues relat*d t* the collection, storage, use and dissemination of patients’ digital health information arise.
The Aadhaar (Hindi, meaning foundation or base) system of India provides each citizen with a unique identification number, linked to demographic and biometric information about
the individual. The National Health Mission established the health management information system across various states of the country, where everyone is also provided with a unique health identification number. Linking this unique health identification number with the Aadhaar system has been *roposed; merging the digital identification system with d*gital health care records could enab*e greater efficiency in investigating public health, conducting relevant research, ensuring the accuracy of health-related information and monitoring welfare
programmes. However, the availability of
big data *n health care, particularly in low- and middle-income countries, introduces unique challenges. We identify and discuss such challenges in this article.
Local setting
The delivery of health care in India is characterized by a vast public health infrastructure, which is categorized into primary, secondary and tert*ary care services, delivered by the government-funded health system and a private health sector. *he public health system is funded by tax revenues and state-sponsored health insurance schemes, such as Ayushman Bharat, and the private health system is largely financed out of pocket and, to a small extent, by private health insurance. In recent years, digital health record* have penetrated the public as well as private health systems; most public *ealth data are now recorded in digital format. One of the major issues faced by the public health sector in India is inadequate funding and inefficient utilization of the
funds allocated. The enhancement of currently available digital health records will greatly increase the efficiency of planning and budgeting for the health care services.
Approach
Under the Unique Identification Authority of India, established under the Ministry of Electronics and Information Technology of the Government of India, the Aadhaar system provides a 12-digit unique identification number to every Indian resident who chooses to enrol as per the provision of the Aadhaar (Targeted Delivery of Financial and Other Subsidies, Benefits and Services) Act, 2016. The Aadhaar identification syste* records demographic data such as name, address, date of birth and sex, but also biometric data including ten fingerprints, two iris scans and a facial photograph*
Identification by Aadhaar number yields several important advantages in development and welfare programmes in the country. Targeted interventions, such as subsidies, cash benefits and incentives provided by the state can reach the intended beneficiaries without pilferage or loss. The Aadhaar system has been increa*ingly linked to bank accounts, income tax accounts, mobile phone numbers, and social welfare programme*, such as disability and elderly pension schemes.
Relevant changes
Since 2013, Aadhaar has *lso bee* linked to
several health-related schemes. For example,
the Maternal and Child Tracking System is an electronic database that records information about pregnant women in India, including details of antenatal care, delivery and child- related data up to immunization. A conditional cash transfer programme (Janani Suraksha Yojna) encourages women to undergo delivery in a health facility by providing a direct benefit transfer; combining this cash transfer programme with the Aadhar identification system ensures that the correct person receives the benefit.
Other national health programmes, such as the Revised National Tuberculosis Control Program and the National AIDS Control Program, have recently started linking their databases with Aadhaar. The intended benefit of linking the patient databases to the Aadhaar number is to track the treatment of patients and ensure that any interruptions to treatment schedules or non-compliance is identified and acted upon. However, interruptions in the treatment of patients with tuberculosis were reported due to pressures to link their treatment registration numbers with their Aadhaar identification number. There have also been several reports of HIV- positive patients and patients with AIDS who were undergoing antiretroviral therapy but, fearing a breach of their privacy by allowing their Aadhaar number to be included in the AIDS treatment programme docu*ents, they preferred to drop out of the treat*ent programme.
The summary of main lessons learnt is presented in Box 1.
Box 1. Summary of *ain lessons learnt
-
 Use of the Aadhaar identification number in health programmes in Indi* has met with mixed success due to patients’ fears of loss of privacy.
Use of the Aadhaar identification number in health programmes in Indi* has met with mixed success due to patients’ fears of loss of privacy. -
 The propo*ed merging of the Aadhaar identification system with other digital health databases in India could enable greater efficiency in monitoring public health, *ut important ethical issues of data use and protection must be considered.
The propo*ed merging of the Aadhaar identification system with other digital health databases in India could enable greater efficiency in monitoring public health, *ut important ethical issues of data use and protection must be considered. -
 Low- and middle-income countries must invest in developing stri*t legal regulations to protect data and avoid its exploitation for profi*.
Low- and middle-income countries must invest in developing stri*t legal regulations to protect data and avoid its exploitation for profi*.
Linking sensitive private health information with the Aadhaar identification system introduces issues of potential breaches of privacy, data ownership and use, and the autonomy of individuals whose data have become available for analysis. Unlike the United Kingdom of Great Britain and Northern Ireland *nd the United States of America, who have strong data ownership and protection laws, India has the evolving Electronic Health Record Standards of 2016, which does not have the force of law. Data are owned by the state in a sense of stewardship in the United Kingdom and by the individual in the USA. The Indian Electronic Health Record Standards stipula*e
Lessons learnt
that data are owned by individuals, but the state is th* custodian of these data. This provision implies that any use of electronic health record* requires the authorization of the individual. The exceptions to this rule are situations of emergency and epidemics, in which case the state can collect information without permission. Where data are shared without consent, this is only in a completely anonymized form.
The Aadh*ar identification system h*s been the subject of several litigations in various courts in India. In a ruling in 2013, the Supreme Court of India clearly ruled that r*gistering for an Aadhaar identification number is voluntary and that nobody should be denied benefits and services because they do not have an Aadhaar number. Despite this ruling, several national health programmes continue to enforce Aadhaar registration in subtle ways. For example, although including an individual’s Aadhaar number is not compulsory in many public health programmes, some health workers continue to insist on this. If patients refuse, the health worker can delay or even prevent the receipt of benefits. In 2017, the Supreme Court ruled that the Right to Privacy is fundamental. This ruling reignited the various debates on the constitutional position of the Aadhaar system and whether it is an infringement of the privacy of individuals. In 2018, the Supreme Court upheld the constitutional position of Aadhaar, but ruled again that it is not mandatory. However, in the absence of strong regulation of electronic health records in low- and middle-income countries, linking sensitive health information to the A*dhaar
system results in the privacy of patients bein* compromised.
Other major ethical concerns regarding the linking of digital health data and Aadhaar identification data are the safety and protection of the combined database. Many low- and middle-income countries do not yet have the required data protection laws; even if such laws are present, implementation can be difficult to monitor. Leaks of the Aadhaar data have been reported; * private telecommunication company in India collected the Aadhaar numbers of many of its subscribers and published them on the internet. Over 200 government websites were also found to be inadvertently displaying
Aadhaar data of individuals. Although these
websites have been taken down, such data can remain in the digital world indefinitely and continue to compromise the privacy of an individual.
Linking digital health data with the Aadhaar
identification system also facilitates the exploitation of the data for profit. Some technologists who were initially involved in
the establishment of the Aadhaar system are
now workin* in private for-profit companies.
Although secu*ity measures are in place to
prevent this conflict of interest, there are
several loopholes in these regulations.
When such profit-motivated, digitally
empowered multinational companies gain
access to an identification database in low-
and middle-income countries, this
disproportionately affects the poor and
vulnerable. Effective security systems and
strong legislation are required to ensure that
private companies do not profit from accessing such databases. In this context, the *inistry of Electronics and Information Technology tabled the Draft Personal Data Protection Bill, 2018. When passed, this bill will set up a national Data Protection Authority to supervise and regulate those who collect data, ensuring the autonomy of individuals.
Low- and middle-income countries are joining the digital revolution, making big data available for potential health applications. However, weak health data protection laws and evolving data protection capabilities in these countries leave the population vulnerable to serious ethical consequences, such as breaches in privacy and loss of autonomy. *n examining the merging of Aadhaar identification data with digital health data in India, we have demonstrated the need for strong health data protection laws to preserve and protect the fundamental human right: that of privacy.
-
1. Wyber R, Vaillancourt S, Perry W, Mannava P, Folar*nmi T, Celi LA. Big data in global health: improving health in low- and middle-income countries. Bull World Health Organ. 2015 Mar 1;93(3)*203–8. http://dx.doi.org/10.2471/BLT.14.139022 pmid: 25767300↩
-
2. Abraham R, Bennett ES, Sen N, Shah NB. State of Aadhaar. Report 2016-17. New Delhi: IDInsight; 2017. Available from:
https://stateofaa*haar.in/assets/download/ State-of-Aadhaar-Report_2016-2017.pdf [cited 2019 Jan 17].↩
-
3. What is Aadhar. New Delhi: Unique *dentification Authority of India; 2019. Available from: https://uidai.gov.in/your- aadhaar/about-aadhaar.html [cited 2019 Dec 2].↩
-
4. Ministry of Law and Justice (Legislati*e Department). The Aadhaar (Targeted Delivery of Financial and Other Subsidies, Benefits and Services) Act. New Delhi: Unique Identification Authority of India; 2016. Available from: https://uidai.gov.in/imag*s/targeted_deliv ery_of_financial_and_other_subsidies_be nefits_and_services_13072016.pdf [cited 2019 Dec 2].↩
-
5. Rao M. Aadhaar made mandator* for TB patients seeking cash assistance from the government. Scroll.in. 2017 Jun 21. Available from: https://scroll.in/pulse/841250/aadhaar- made-mandatory-for-tb-patien*s-seeking- treatment [cited 2019 Dec 5].↩
-
6. Rao M. Why Aadhaar is prompting HIV positive people to drop out of treatment programmes across India. Scroll.in. 2017 Nov 17. Avail*ble from: https://scroll.in/pulse/857656/across- india-hiv-positive-people-drop-out-of- treatment-programmes-as-centres-insist- on-aadhaar [cited 2019 December 2].↩
-
7. Electronic health record (EHR) standards for India. New Delhi: Ministry of Health
https://mohfw.gov.in/basicpage/electronic -health-record-ehr-standards-india-2016 [cited 2019 Dec 2].↩
-
8. Safi M. Indian court upholds legality of world’s larg*st biometric database. The Guardian. 2018 Sep 26. Available from: https://www.theguardian.com/world/2018/ sep/26/indian-court-upholds-legality-o** worlds-largest-biometric-database [cited 2019 Dec 2].↩
-
9. Press Trust of India. Over 200 govt websites made Aadhaar details public: UIDAI. The Times of India. 2017 Nov 19. Available from: https://timesofindia.indiatimes.com/india/ 210-govt-websites-made-public-aadhaar-
details-uidai/articleshow/61711303.cms [cited 2019 Aug 22].↩
-
10. Thaker A. The new oil: Aadhaar’s mixing of public risk and private profit. The Caravan. 2018 May 1. Availa*le from: https://caravanmagazine.in/*eportage/aadh aar-mixing-public-risk-private-profit [cited 2019 Dec 2].↩
-
11. The Personal Data Protection Bill. New Delhi: Ministry of Elect*onics and Information Technology; 2018. Available from: https://meity.gov.in/writereaddata/files/Pe rsonal_Data_Protection_Bill,2018.pdf [cited 201* Dec 2].↩

Issue: Volume 4, Issue 2
Paradigm *hift in Cancer M*nagement - Molecular Therapy
Dr *oonam Patil (Consultant Medical Oncologist at Manipal Hospitals, Bangalore)
National C*ncer Institute defines molecular therapy in cancer treatment as substances that kill cancer cells by targeting key molecules involved in cancer cell growth.
The need for targeted therapy in cancer was realized long back when undesirable side effects of chemotherapy were seen. This was a dream of having a treatment specifically directed towards functionality at level of cancer cell with minimal toxicity to normal host tissues. Paul Eh*lich’s vision of “magic bullet” in cancer therapy is being realized now.
Cancer cells are recognized to have specific antigenic and molecular receptors as the starting point for a cascade of events leading to cell *ivision, and specific enzymes triggerin* cell division and angiogenesis. Most of the molecular therapy measures are directed against these targets.
Targeted therapy includes two arms – what to target and how to target ( receptor function
and delivery function). It encompasses several classes of agents like m*noclonal antibodies and tyrosine kinase(TK) inhibitors. Molecularly targeted therapy has used both small molecules to directly inhibit these TKs and monoclonal antibodies to indirectly affect the pathways these TKs control.
Cancer care has advanced in the last decade in leaps and bounds by improving treat*ent, early detection and prevention.
Traditional chemotherapy looked at killing the cancer cell directly as a bombing action. Newer agents kill cancer cells like missile action, targeting only the cancer cells, though there are some associated side effects on normal cells.
Newer agents can be classified into two -
Targeted therapy - may either attack tumor cells directly or, by stimulating the immune system, target them indirectly.
If we look at the genetic make up of the
tumor regardless of the site of tumor, and give treatment targeted according to the unique molecular profile of the malignancy, it is known as precision medicine or personalized medicine. This complex but unique molecu*ar profile can be studied now, by tests known as Next gene*ation sequencing.
Biological therapy – Biological therapy involves the use of living organisms, substances derived from living organisms, or laboratory-produced versions of such substances to treat disease
Targeted therapy
The era of personalized *edicine actually started many years back when the drug Tamoxifen was used to treat Estrogen receptor positive breast c*ncer cells. However it was m*ch later that the knowledge of the biological functioning of a cell was understood and many targets identified. The first drug of this era was Imatinib in 2001, which targeted the bcr-abl oncogene which resulted due to Philadelphia chromosome in patients with Chronic myeloid leukemia. The BCR-ABL chimeric fusion protein *auses tyrosine kinase activity which causes uncontrolled cellular proliferation, which was inhibited by Imatinib. This drug has stood the test of time and has made it possible for many patients of Chronic myeloid leukemia to enjoy long term survival, and possible cur* for a small subset of patients.
Such drugs are known as “small molecule tyrosine kinase inhibitors”. These drugs may
interfere wi*h a specific protein function, which has Tyrosine kinase activity which c*uses uncontrolled cell proliferation. These drugs are not derived from biologic sources and hence do not come under classification of biological therapy or immunotherapy.
Some examples of small molecules interfering with intracellular signal transduction:
Against EGFR (epidermal growth factor receptor)
Erlotinib, Lapatinib (dual), Gefitinib
Against VEGFR (vascular endothelial growth factor receptor)
Sorafenib
PDGFR (platelet derived growth factor receptor)
Imatinib, Sunitinib, Afatinib
Examples of some drugs and the*r use :
|
INN Indication |
|
|
Tyrosine kinase inhibition |
|
|
imatinib |
CML, GIST |
|
dasatinib |
CML |
|
gefitinib |
NSCLC, ORL |
|
erlotinib |
NSCLC |
|
semaxanib |
Colorectal Ca |
|
lapatinib |
RCC, Breast Ca, H + N |
|
sorafenib |
Liver Ca |
|
Proteasome inhibition (multi catalytic protease complex) |
|
|
bortezomib Multiple myeloma, NHL |
|
Another fine example of targeted therapy associated with a specific genetic mutation is seen in patients with breast and ovarian cancers. It has been found that BRCA gene is mutated in a minority of patients with ovarian and breast cancer. Now BRCA gene is actually a tumor suppressor gene which helps in repairing damaged DNA (double stranded DNA breaks) by error free homologous recombinant repair. If BRCA gene is mutated, it is unable to perform its function of DNA repair. This is where an enzyme named PARP - Poly (ADP-ribose) polymerase, a family of proteins involved in a number of cellular processes such as DNA repair comes into play. PARP is a protein that is important for repairing single-strand breaks. Now if BRCA is mutated, then PARP comes and repairs the damaged DNA in cancer cell. If this PARP is inhibited, then the DNA in cancer cell has no way to repair itself and it dies. The PARP inhibitors used in treatment of BRCA mutated ovarian and breast cancers are Olaparib, Talazoparib. They have been used in various settings – first line, second line or even third
lines of therapy of BRCA mutated cancers of ovary. Besides cancers of breast and ovary, BRCA mutations have been seen in Prostate and Pancreatic cancers and these drugs have been used in them.
Biological therapy
This involves usage of an antibody against a target antigen seen on the tumor cell. Since the antibodies are made in laboratory using living organism, they are known as biological therapy. Also as this involves *n antigen- antibody interaction, they are also known as immunotherapy.
Terminology of monoclonal antibodies
Murine monoclonal antibodies – high production of HAMA; generic ending: -mab.
Chimerical monoclonal antibodies – 60–70 % of human protein (constant domains) + 30– 40 % murine antibodies; generic ending: - ximab.
Humanized monoclonal antibodies – 5–10 * murine antibodies; generic ending: -zumab
Human monoclonal antibodies (100% human); generic ending: -mumab
Immunotherapy is again of several types:
1. Identifying target antigen on cancer cell and an antibody produced against it – eg Anti CD 20 antibody Rituximab for CD 20 positive B cell lymphomas, anti Her 2
neu antibody Trastuzumab for Her 2 neu positive breast cancer.
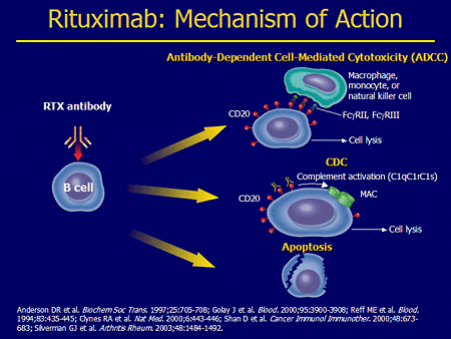
Also now, an*ibody drug conjugates are available – in which the antibody is linked to a cytotoxic drug. The presence of antibody helps in gaining entry of the conjugate into the cancer cell, and once it enters, the drug is released inside the cancer cell, where it can disrupt various cell functions killing the cancer cell. Drugs available are Ado –trastuzumab (Her 2 neu positive breast cancer), Brentuximab vedotin (CD30 positive Hodgkins lymphoma).
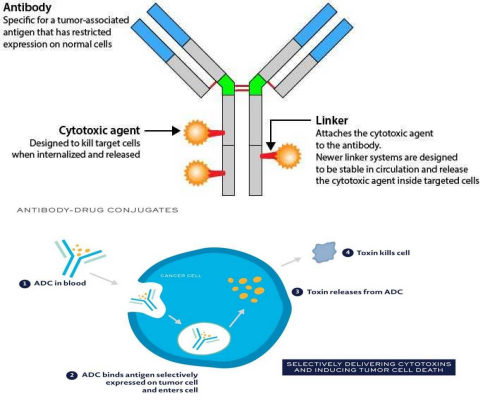
-
2. Immune check point inhibitors – this is the most recent development in treatment of cancers. It has been long understood
that our immune system, especially T lymphocytes, has the capability of identifying and killing cells “foreign” to the body. The immune system is however kept under check by “check point inhibitors” as the T lymphocytes can also mount an auto immune “response which is detrimental to body. In many diseases including cancers, this ability is lost due to multiple reasons. One such proposed reason is that the cancer cell has suppressors which suppress the T lymphocytes.
-
3. Targeting tumor angiogenesis –As the cancer cells increase in size and number, they eventually require their own blood supply to keep them growing. They do so by secreting cytokines which results in neo-a*giogenesis. It has been in scientific experiments since many years that if the tumor could be somehow starved, it will not grow. A lot of work was carried on by Dr Judah Folkman in this field. Bevacizumab is a humanised recombinant antibody that prevents vascular endothelial growth factor (VEGF) receptor binding, and inhibits angiogenesis and tumour growth.
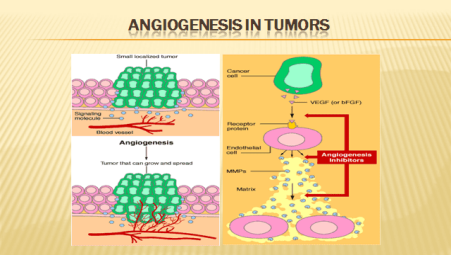
-
4. CAR (chimeric antigen receptor) T cells where there is reprogramming and
expansion of a T cell clone in vitro which is then injected back into the host, where these T cells then kill the cancer cell – activity seen in lymphomas.
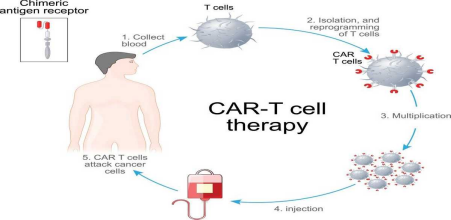
5. Va*cine therapy – sipuleucel-T is an FDA approved personalized therapy against prostate cancer. It can activate patient’s own immune system to seek out and attac* advanced prostate cancer. First the patient’s blood is run through a pheresis machine when some of the patient’s immune cells are collected. These immune cells are then expos*d to a protein intended to stimulate and direct them against prostate cancer. Following
this e*posure, the activated immune cells ar* then returned to the patient to treat the prostate cancer. In addition to the antigen presenting cells, it also contains T cells, B cells, natural killer (NK) cells, and other cells.
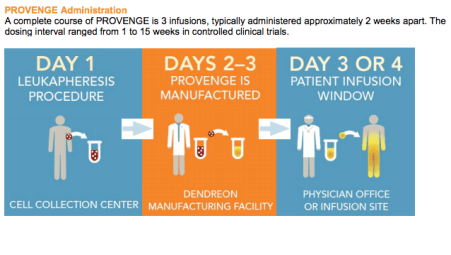
These are some of the new advances which have changed our mindset towards treating cancer. Looking into the future, all malignancies will be a*sessed for targets and genetic mutations and treated accordingly.

Issue: Volume 4, Issue 2 News
Spice Route India Cafe: Voices of Young Family doctors from across the country
Swathi S B (Primary Care Physician and Researcher; Lead, Karnataka Chapter, Spice Route India)
On the occasion of World Family Doctors’ day, young family doctors from across the country met on a virtual platform at Spice Route India cafe, to share their experien*e about providing Primary Health Care during the challenging situation of the current COVID-19 pandemic. This event was organised by Spice Route India under the leadership of Dr Serin Kuriakose, Dr Jyotika Gupta, Dr Kailas P, Dr Mohammed Idris and state leads on May 17, 2020 from 9:00 - 11:00 pm.
Spice Route India is a young doctors movement under the aegis of AFPI. And this event was first of its kind in its history.
This also marked the pleasant inauguration of the Spice Route India website by National Vice President AFPI, Col. (Dr) Mohan Kubendra. Link to the website : https://spiceroute.afpikerala.in/
More than 70 doctors participated in the cafe and family doctors from 11 states of India shared their personal experience in caring for patients during COVID 19. Participants were from across the country - spanning from Rajasthan to Nagaland and Haryana to Kerala - and included senior physicians ,young family medicine post graduates and MBBS students as well. Not to forget, we had our guests and colleagues from Sri Lanka and Bangladesh too, as a part of Spice Route SAR.
Varied experiences were shared. Running private clinics with precautions, using tele- medicine as triage, working in the public health sector, attending to COVID pat*ents in the ICUs, to name a few.
Dr Piyush Jain, member of National Executive AFPI and Nodal officer at District hospital, Agra ,was the chief guest and he *rought to light the challenges in careful
management of chronic illness and non- communicable diseases during pandemic.
All in all, it was refreshing to take a pause and reflect on our practices, emotions, behavioural changes that our patients and we practitioners are goin* through, and what to expect going forward. It also brought the sense of collective learning and togetherness among the warriors in the current battle!