AFPI kARNATAKA newsletter

Case Series
Experience
AFPI News
Clinical Updates
Articles
Letters
AFPI Karnataka Quarterly Newsletter� - Vol. 7 issue: 4 - 15 October 2024
Contents.
4. AFPI news
5. Events
7. Articles
a. Three Stage clinical assessment. A case series
b. Monoclonal Gammopathy of Undetermined Significance (MGUS): an overview
c. Transient elastography/ Fibroscan in clinical practice: A physician�s guide
d. Recurrent Hypokalemia induced by Primary Aldosteronism due to Unilateral
8. Case report
(Please click the title to follow the link)
We strive� every day to build a healthier and more prosperous environment around us , and I want to emphasize the vital role of family medicine doctors in shaping the future of our healthcare system.
Family medicine doctors are the backbone of our healthcare infrastructure, providing primary care to millions of Indians every day. We are the first point of contact for patients, offering compassionate and comprehensive care that addresses the unique needs of each individual and family.
As we move forward, I envision a healthcare system where family medicine doctors are empowered to take on even greater responsibilities. They will be/are� the leaders of healthcare teams, coordinating care and ensuring that patients receive seamless and high-quality cost-effective treatment. They are now everywhere, from remote areas to metro cities, in clinics elderly care homes, day care centers , diagnostic centers ,small hospitals to quaternary care centers ...In all these centers, people come for their family doctors and other specialty experts have started looking up and relying on family medicine specialist ! World's vision on family medicine is changing and the TRUST is coming back.
To sustain this vision and nurture it further, we must invest also in the training and development of our family medicine doctors, providing them with the skills and resources they need to thrive in an ever-changing healthcare landscape.
Let us recognize the critical role that family medicine doctors play in building a healthier India and commit to supporting them every step.
With best wishes,
Dr Sowmya B Ramesh
Dr Sowmya B Ramesh
President, AFPI Karnataka
On behalf of the Academy of Family Physicians of India (AFPI) Karnataka, it is my great pleasure to introduce the newly elected members of the Executive Committee (EC) for the 2024-2026, following the recent elections held on 1st September 2024. These accomplished professionals bring a wealth of knowledge, leadership experience, and dedication to advancing the cause of family medicine in India.
The newly elected Executive Committee members are:
1. Dr Sowmya B Ramesh, President 9900966617, drsowvivek@gmail.com
2. Dr Harshapriya Jyothinagar, Vice President drharshapriyaj@gmail.com
3. Dr Hemavathi Dasappa, General Secretary 9902872666, hema.dkp@gmail.com)
4. Dr Supritha K M, Treasurer 9353425411, dr.supz23@gmail.com)
5. Dr Madhumitha R Member 8376045421, rmadhumitha13@gmail.com)
6. Dr Vinod Babu Veerapalli, Member Executive 9036457134, drvvinodbabu@gmail.com)
7. Dr Impana G N, Member 8593091822, gn.impana@gmail.com)
8. Dr Amrutha J H, Member 9535650699, dr.amruthajh2128@gmail.com)
9. Dr Naveen Kumar Pathalapati, Member (Executive ) (9985489787, Naveen.doctor27@gmail.com)
I am confident that this new team will further strengthen the role of family physicians in providing comprehensive healthcare and will contribute significantly to the growth of our academy. We are also committed to working closely with the journal and other stakeholders to highlight the importance of primary care and to foster academic contributions in this field.
The Karnataka Chapter has always been at the forefront of promoting primary care and strengthening the role of family physicians in providing holistic healthcare services. Under our tenure, we plan to further our efforts in continuing medical education, fostering collaborations with healthcare institutions, and advocating for policy reforms that empower family physicians.
We also look forward to working closely with AFPI members across the country, sharing our experiences and knowledge through various platforms, including this esteemed journal. It is my firm belief that through collective effort and consistent engagement, we can address the evolving healthcare needs of our society and fortify the foundations of primary care.
I would like to take this opportunity to extend my sincere thanks to the AFPI leadership and my fellow colleagues for placing their trust in us. We are committed to serving the academy and our members to the best of our abilities.
We look forward to the continued support and guidance from the AFPI community as we embark on this journey together.
Yours sincerely,
Dr Hemavathi D
Dr Hemavathi D,
Hon Gen Secretary, AFPIKA
There has been a change of guard and the new set has taken over the functioning of the Karnataka branch of the academy of family physicians of India. Founder president of Karnataka chapter, Col Mohan Kubendra has assumed charge as the president of the central body. Most people working in the field of health which includes medical education and health care delivery are aware of the fact that the present system of educating the doctors and delivery of care has major defects waiting to be remedied. Neglect of primary care and public health at the cost of over emphasis on curative medicine over the past several decades has led to a scene where there is inequitable health care delivery.
While it is true that world class health care is available to some sections of the society, it is also true that large sections remain deprived of quality health care. It is time we devout more resources to provide efficient primary care, preventive and promoting health.
It is my hope Academy of family physicians of India, under the dynamic leadership of Col Mohan Kubendra will prove to be an effective influencer towards achieving goal.
B.C Rao
Badakere.rao@gmail.com
Chief Editor

Let us welcome our new National Executive. Our new executive brings a wealth of experience, passion, and vision that aligns seamlessly with our core values.
Dr (Col.) Mohan Kubendra - National President
Dr Vandana Boobna - National Vice-president
Dr Resmi S Kaimal -National General secretary
Dr Serin Kuriakose-National Treasurer
Executive members
Dr Jyotika Gupta
Dr Kiranmayi Lingutla
Prof (Dr) Venkatesan Pandian
Gp Capt (Dr) Abhijit Mandal




Memorandum of Understanding (MoU) between AFPI (Academy of Family Physicians of India) and FFPAI (Federation of Family Physicians' Associations of India) is a pivotal step towards formation of a Unified front by synergizing their strengths and advancing family medicine in India. Both organizations aim to elevate the standards of primary care, support professional development, and positively impact healthcare delivery across the country through collaborative efforts.
The Spice Route India Movement, Karnataka Chapter Achieves Milestone in PG Exam Orientation
The Spice Route India Movement, Karnataka Chapter, successfully conducted two Post Graduate Exam Orientation (PEOS) sessions in Bengaluru, in collaboration with Trustwell Hospital and Bangalore Baptist Hospital, in February and August. These sessions aimed to train and orient postgraduate students for their practical exams.
The initiative received an overwhelming response from pan-India, with over 100 students benefiting from the sessions. We take pride in having instilled confidence and empowered these students to excel in their exams.



Recent CME Highlights
September Session: Heart & Gut Innovations : Pioneering Advances in Cardiology and Gastroenterology
Our September CME session spotlighted crucial topics in cardiology and Gastroenterology, offering actionable insights for early recognition and management in primary care:
Heart Failure: Early Recognition and Management
The session emphasized key alerts for detecting heart failure early, enabling prompt and effective intervention by primary care physicians.
Post-MI Rehabilitation: Road to Recovery
We explored comprehensive rehabilitation strategies following a myocardial infarction, ensuring optimal recovery for patients in a primary care setting.
Newer Diagnostic Techniques in Cardiology
An engaging discussion on the use of CT Coronary Angiography and Calcium Scoring provided clarity on when these diagnostics are necessary and their relevance in modern practice.
What�s New in Dyslipidemia Management
A deep dive into recent advancements in managing dyslipidemia, updating participants on new therapeutic approaches to optimize lipid levels.
Fatty Liver: Diagnosis and Management
We provided updated guidelines for diagnosing and managing fatty liver, equipping physicians with modern tools and approaches to tackle this rising concern.
Vitamin B12: Symptoms, Testing, and Supplements
A thorough panel discussion covered the often-overlooked symptoms of Vitamin B12 deficiency, the importance of appropriate testing, and the range of supplements available for different clinical needs. As we continue to reflect on these informative and impactful sessions, AFPI Karnataka remains committed to supporting continuous professional development and fostering a collaborative environment for all. Stay tuned for upcoming initiatives as we strive to advance medical education across the region!
Annual general body meeting
Highlights of the AFPI Karnataka Annual General Body Meeting (GBM)
On 1st September 2024, AFPI Karnataka successfully conducted its Annual General Body Meeting (GBM), attended by approximately 25 active members. The meeting marked a significant milestone for the organization, reinforcing our commitment to advancing the field of Family Medicine and Primary Care. The proceedings began with a presidential address by Dr. R.K. Prasad, who highlighted the organization's accomplishments over the past year and emphasized the collective responsibility of members to continue striving towards excellence in primary care education and practice.

Following this, Dr. Harsha Priya, General Secretary, presented a comprehensive Activities and Accomplishments Report, detailing AFPI Karnataka�s initiatives over the past year. These included CME sessions, workshops, community outreach programs, and collaborative efforts with healthcare institutions, all designed to promote the role of Family Medicine in improving patient outcomes.
Dr. Gowri Chinthalapalli, Treasurer, delivered the Finance and Audit Report, providing a transparent overview of the organization�s financial health. The report underscored the judicious use of resources in organizing educational programs and ensuring the financial sustainability of the association.
A key highlight of the GBM was the Executive Committee Restructuring. After careful deliberation, a new Executive Committee was inducted, which will lead the organization for the next two years, serving until 2026. The newly appointed office-bearers are as follows:
President: Dr. Sowmya B. Ramesh
Vice President: Dr. Harsha Priya Jyothinagar
General Secretary: Dr. Hemavathi D
Treasurer: Dr. Supritha K M
In addition, the following individuals were inducted as Executive Committee
Core Members:
Dr. Impana
Dr. Vinod Babu
Dr. Amrutha
Dr. Naveen
Dr. Madhumita
The GBM concluded with a renewed sense of purpose and unity, as members committed to the continued growth and success of AFPI Karnataka in its mission to empower family physicians and improve healthcare delivery in Karnataka. We look forward to the contributions of the new leadership team as they guide the association into the future
We are excited to invite you to WONCASAR 2025 (World Organization of Family Doctors - South Asia Region Conference), taking place from April 4-6, 2025, in Bangalore, INDIA.

This premier event will unite leading family doctors, researchers, and healthcare professionals to explore the latest advancements and best practices in family medicine. Secure your spot by registering before the early bird deadline on December 31, 2024, to take advantage of special rates. For more details and to register, please visit our conference website [www.woncasarindia2025.com].
We look forward to seeing you there!
The new name for Non-alcoholic steatohepatitis (NASH) has been renamed to Metabolic Dysfunction-Associated Steatohepatitis (MASH).
This change was made to better reflect the metabolic nature of the disease and to avoid confusion with alcoholic liver disease.
Non-alcoholic fatty liver disease (NAFLD) has also been replaced by metabolic dysfunction-associated steatotic liver disease (MASLD).

The 2021 American College of Cardiology and American Heart Association guidelines no longer recommend classifying chest pain as atypical or typical, because this classification is not useful for identifying the cause and has been misused to classify chest pain as benign. Instead, the guidelines now recommend that chest pain be classified as cardiac, possibly cardiac, or noncardiac
Medical management of acute coronary syndrome (Apart from antiplatelets)
|
Medication |
Special indications |
Daily target Dose |
Contraindication |
|
Statins |
Recommended for all patients |
High-intensity dosing: atorvastatin 40 or 80 mg; rosuvastatin 20 or 40 mg |
Active liver disease or severely elevated liver transaminase levels (> 3 to 5 times the normal limit) |
|
Ezetimibe |
Consider in patients already on maximally tolerated statin dose with low-density lipoprotein > 70 mg per dL (1.81 mmol per L) |
10 mg A |
Active liver disease |
|
Beta blocker |
Recommended for all patients; consider strongly if reduced LVEF |
Various; consider stopping after 2 to 3 years if patient has adverse effects and no other indications |
Second- or third-degree heart block, severe bradycardia |
|
ACE Inhibitors /ARBs |
Consider if patient has reduced LVEF or diabetes mellitus; ARB/ neprilysin inhibitor may be preferred if LVEF < 40% |
Various |
History of anaphylaxis or angioedema |
|
Mineralocorticoid receptor antagonists |
Consider if LVEF < 40% |
Spironolactone 12.5 or 25 mg; eplerenone 25 or 50 mg |
Potassium level > 5.5 mEq per L (5.5. mmol per L) or CrCl < 30 mL per minute |
|
SGLT2 inhibitors |
Consider for all patients; consider strongly for those with diabetes or heart failure regardless of LVEF |
Empagliflozin (Jardiance) 10 or 25 mg; dapagliflozin (Farxiga) 5 or 10 mg |
CrCl < 45 mL per minute for dapagliflozin; CrCl < 30 mL per minute for empagliflozin |
|
GLP -1agonist |
Consider if patient has diabetes |
Various |
Medullary thyroid cancer, multiple endocrine neoplasia type 2, pancreatitis |
Three-stage clinical assessment �
A case series
Background
���������� In the traditional method of clinical assessment, we take history, examine the patient,
come to a provisional diagnosis, investigate, and treat. In this traditional method the disease is the centre of care.
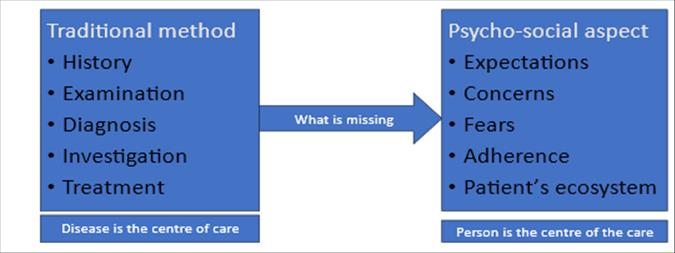
Fig 1: Background
What we are missing in the traditional method is the psycho-social aspect which is patient�s expectations, concerns, fears, adherence to medications and ecosystem. Including psychosocial aspect in the care of the leads to patient centered care where patient is the center of care.
�Patient-centered care that encompasses informed decision making can improve treatment choice, quality of care and outcomes. It recognizes the need for major changes in the process of care that arranges health care system around the patient. It may provide solutions to several pressing problems like cost of services, poor outcomes of chronic care etc. In complex health settings, coordination and cooperation are often absent within and across levels of service, between facilities and across sectors.
�Partnership approach is the most important aspect of three-stage clinical assessment.� In this Doctor, who diagnose, treat and prevent the disease and patient with his/her context, habits and preferences, share information, negotiate and come to a joint decision. Three-stage assessment helps the patient and the physician to deal holistically with the problem and to individualize the assessment and management.
University of Medusa, Republic of South Africa proposes three stage assessment, based on two articles published by Mc Whinny�s in 1969 on three stage diagnosis and Stott and Davis in 1979. The three-stage assessment which includes clinical, individual and contextual assessment is person centred clinical method.
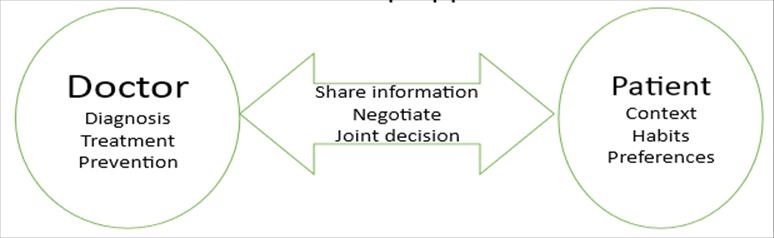
Fig 2; Partnership approach
|
Three stage assessment |
||
|
1st�Stage |
Clinical assessment |
History, examination, Investigation |
|
2nd Stage |
Individual assessment |
Fears, concerns, ideas and expectation |
|
3rd�Stage |
Contextual assessment |
ECO-Mapping |
In this article we will describe use of three stage assessment method using three case scenarios.
The stages of clinical assessments are,
1st stage (Clinical) � History, physical examination, investigations.
2nd stage (Individual) - Concerns/fears / ideas of the patient about his/her symptoms and his/her expectations.
3rd stage (Contextual) - How does the disease affecting his/her life? How does his/her life affected by the disease? and eco mapping.
Case 1 � 27 years old male who presented with pancytopenia and Vit B12 deficiency. His Hb was 5 gm%. He had done doctor shopping. He was living with his parents. His 2 siblings were already married and living separately.
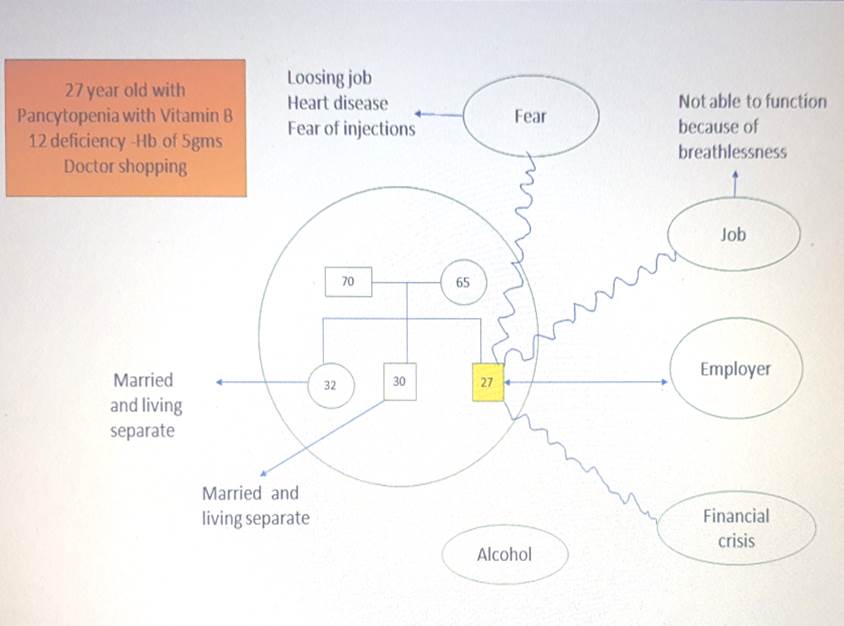
Fig 3; Case 1
|
Assessment |
Plan |
|
|
Contextual |
Runs a business �under loss and going through major financial crisis Does not share his problems with family Not compliant to the treatment |
Limited investigation Changed to low cost medicine |
|
Individual |
Thinks that there is some major cause for uncontrolled BP |
Reassured and to review again once compliance is achieved |
|
Clinical |
Uncontrolled BP � |
Prescribed low cost medicine Emphasised the need for compliance |
|
Next visit his BP was 150/90mmg |
||
Assessment � Contextually, runs a business �under loss and going through major financial crisis. He does not share his problems with family, not compliant to the treatment. Clinically, Uncontrolled BP. Individually, he thinks that there is some major cause for uncontrolled BP.
Plan - Resource is friend, who shared most of his friend�s problem and he was communicating with us instead of patient. Requests for generic medicine. Limited investigations and changed to low-cost medicine. We emphasised the need for compliance. We reassured and to review again once compliance is achieved.
Follow up � compliance was achieved and BP was 150/90 mmHg.
Discussion
Three stage clinical assessments yielded essential details about patient�s varied and multimorbid conditions, while personal and contextual assessments highlighted issues that put patient�s care needs and possibilities into perspective. All the assessments were combined to make patient-tailored action plan and applied them by facilitating cooperation through inter professional and inter sectoral networks.
���������� Compliance to treatment achieved. Generic medicines were prescribed wherever it was necessary. Relevant investigations and treatment expenses were met by the benefactors like family members, friends, employer at the request of the treating physician. Hence, it was cost effective than traditional method. End result was satisfying to both physician and the patient.
What difference does this make?
- Compliance to treatment is achieved
- Mutually acceptable assessment and plan.
- It solves previously insoluble problems.
- It can be more satisfying for doctor and patient
When to use?
-Undifferentiated illness
-Diagnosis of chronic disease
-Diagnosis of disease of major concern-Anaemias, Infections etc
-Unhealthy habits/High risk behaviors
-Mental illness
-Geriatric patients
Conclusion :
The conceptual model of three-stage clinical assessment helped in improving patient care. Hence this method can be adopted in Family Medicine clinical practice.
Reference :
Hugo, J.F.M., Maimela, T.C.R., Janse van Rensburg, M.N.S., Heese, J., Nakazwa, C.E. & Marcus, T.S., 2020, 'The three-stage assessment to support hospital-home care coordination in Tshwane, South Africa', African Journal of Primary Healthcare & Family Medicine 12(1), e1-e10.
Dr Hemavathi D
Dr Shaini Joyce
Department of Family medicine,
St John�s medical college
Introduction
Monoclonal Gammopathy of Undetermined Significance (MGUS) is a condition characterized by the presence of a monoclonal protein (M-protein) in the blood, produced by a small number of abnormal plasma cells. It is a clinically asymptomatic premalignant clonal plasma cell or lymphoplasmacytic proliferative disorder. While MGUS is generally benign and asymptomatic, it is considered a precursor condition that can progress to more serious plasma cell disorders, such as multiple myeloma, Waldenstr�m's macroglobulinemia, or amyloidosis. Understanding when to suspect MGUS, how to diagnose it, and the current management strategies is essential for clinicians to manage patient outcomes effectively.
Epidemiology
Exact incidence and prevalence of MGUS in India is not known, one of the study determined The overall prevalence of MGUS was 1.43% in the evaluated Indian cohort, lower than that reported for white and black populations (1). MGUS was found in approximately 1 to 2 percent of adults in studies from Sweden, the United States, France, and Japan. The mean age at diagnosis is 70 years, and less than 2 percent of individuals are diagnosed before the age of 40 (2, 3) The incidence and prevalence rises with individual age
Genetic predisposition�
�Most cases of MGUS appear to be sporadic, relatives of individuals with MGUS or other plasma cell disorders have an increased risk of developing MGUS and related diseases (4, 5) It is likely there is� shared environmental and/or genetic predisposition to these disorders.
When to suspect MGUS?
Clinical Presentation
MGUS is usually asymptomatic and is often discovered incidentally during routine blood tests or evaluations for other conditions. Most individuals are identified when an M protein is detected as an incidental finding on protein electrophoresis, performed as part of an evaluation for one of a wide variety of clinical symptoms and disorders
Most individuals are identified when an M protein is detected as an incidental finding on protein electrophoresis performed as part of an evaluation for one of a wide variety of clinical symptoms and disorders such as those with, peripheral neuropathy, vasculitis, hemolytic anemia, skin rashes, hypercalcemia, elevated erythrocyte sedimentation rate.
Largely MGUS is asymptomatic, the condition is likely to have existed in an undetected state for years prior to diagnosis.
Monoclonal proteins
The M protein usually presents as a single narrow peak, like a church spire, in the gamma, beta, or alpha-2 region of the densitometer tracing. Serum immunofixation confirms the presence of an M protein and determines its type
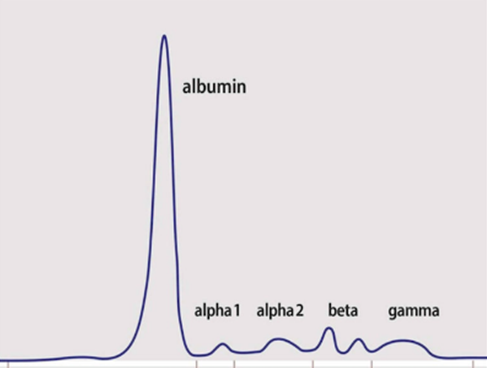
Fig 4: Normal serum electrophoretic pattern
Plasma cells produce immunoglobulins, which are heterodimeric proteins composed of two heavy and two light chains. They can be separated functionally into variable� domains that binds antigens, and constant domains that specify effector functions such as activation of complement or binding to Fc receptors. Immunoglobulins target and neutralize specific threats to the body such as bacteria and viruses.
Plasma cells normally produce some excess light chains that do not combine with heavy chains and instead enter the bloodstream. Free light chains (FLC) or serum free light chains (SFLC) refer to those that are not part of whole (intact) immunoglobulins and are present in the blood.
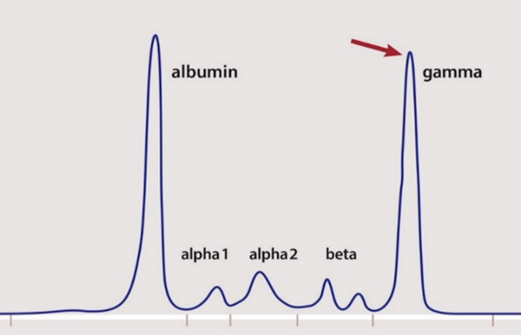
Fig 5: Monoclonal paraprotein in gamma region with church spire like shape in multiple myeloma
�The clonal plasma cells in multiple myeloma and other plasma cell disorders can produce immunoglobulin heavy chains plus light chains or light chains alone, with the following approximate frequencies ( 6,7,8)
� IgG � 55 percent
� IgM � 14 percent
� IgA � 9 percent
� IgD � <1 percent
� Biclonal � 3 percent
� Kappa or lambda light chain only (no heavy chain) � 19 percent
� Kappa light chain � 62 percent
� Lambda light chain � 38 percent
Risk factors
Certain populations are at a higher risk of developing MGUS:
Age: The prevalence of MGUS increases with age, especially in individuals over 50.
Gender: MGUS is more common in males than females.
Race: African Americans have a higher prevalence of MGUS compared to Caucasians.
Family History: A family history of plasma cell disorders increases the risk of MGUS
How to diagnose MGUS?
Laboratory Testing
The diagnosis of MGUS typically involves several key laboratory tests:
Complete blood count
Serum calcium
Serum creatinine
Serum Protein Electrophoresis (SPEP): This test detects and quantifies the M-protein in the blood. It is the cornerstone of MGUS diagnosis.
Immunofixation Electrophoresis (IFE): IFE is used to confirm the presence and type of monoclonal protein (IgG, IgA, IgM, etc.).
Serum Free Light Chain (FLC) Assay: This test measures the kappa and lambda light chains in the blood, helping to assess the ratio, which can be abnormal in MGUS.
Diagnostic criteria
The following criteria are used to diagnose MGUS:
Serum M-protein level < 3 g/dL.
Bone marrow plasma cells < 10%.
Absence of end-organ damage (hypercalcemia, renal insufficiency, anemia, or bone lesions), which would suggest a more serious condition such as multiple myeloma.
Absence of other diseases that can produce similar monoclonal proteins, such as amyloidosis, Waldenstr�m's macroglobulinemia, Lymphomas
Current management of MGUS
Risk Stratification
Once MGUS is diagnosed, the risk of progression to a malignant condition needs to be assessed. The Mayo Clinic risk model is commonly used and considers three factors:
1.���� Non-IgG isotype (e.g., IgA or IgM).
2.���� Serum M-protein level ≥ 1.5 g/dL.
3.���� Abnormal FLC ratio (<0.26 or >1.65)
The normal range for the FLC ratio is 0.26�1.65.
The free light chain (FLC) ratio is a measure of the levels of kappa and lambda light chains in the blood, and it can help diagnose monoclonal gammopathy (MG):
Patients are stratified into low, intermediate, or high risk based on these factors.
�Risk of progression to malignancy
�Individuals with non-IgM MGUS are at risk for progression to smoldering MM (a more advanced premalignant stage) and to symptomatic MM. Less frequently, these individuals progress to plasmacytoma, Amyloid light chain amyloidosis, or related plasma cell malignancy. Besides progression to malignancy, patients with MGUS can also develop a variety of nonmalignant disorders that are related to the effect of the paraprotein on organs such as the kidney, skin, and peripheral nerves. These disorders, which are related to the unique characteristics of the paraprotein, are sometimes collectively referred to as monoclonal gammopathy of clinical significance to indicate that MGUS can cause clinical problems even without progression to malignancy.
Individuals with non-IgM MGUS progress to more advanced disease at a rate of approximately 1 percent per year� (9, 10,11).
For most patients with MGUS, active treatment is not required. Instead, regular monitoring is essential:
Low-risk MGUS: Follow-up every 6-12 months with repeat blood tests (SPEP, FLC assay, and complete blood count).
Intermediate-risk and high-risk MGUS: More frequent follow-ups, usually every 3-6 months, may be warranted.
During these follow-ups, clinicians monitor for signs of progression, such as an increase in M-protein levels, changes in FLC ratio, or new symptoms suggestive of end-organ damage.
Lifestyle and preventative measures
Patients with MGUS should be encouraged to:
Maintain a healthy lifestyle, including a balanced diet and regular exercise, to minimize other health risks.
Avoid factors that may stress the kidneys, such as dehydration or nephrotoxic drugs.
Stay informed about potential symptoms of progression and report any new symptoms promptly.
Research and emerging therapies
While there is currently no treatment to prevent the progression of MGUS to multiple myeloma or other malignancies, ongoing research is focused on identifying biomarkers and potential therapeutic interventions that may alter the course of the disease. Clinical trials are on exploring the use of medications such as bisphosphonates, immunomodulatory drugs, and monoclonal antibodies in high-risk patients, but these are not yet standard care.
Conclusion
MGUS is a common and often benign condition, but it requires careful monitoring due to its potential to progress to serious plasma cell disorders. Early identification, accurate diagnosis, and appropriate risk stratification are crucial for managing MGUS. Regular surveillance and patient education are the mainstays of management, with emerging research offering hope for future therapeutic options. As our understanding of MGUS continues to evolve, so too will the strategies for managing this precursor condition.
Dr Mallikarjun Kalashetty
mkalashetty@gmail.com
Dr Asish Dixit
adxt001@gmail.com
Department of Hemato Oncology
Manipal hospitals
References
1. Gupta R, Dahiya M, Kumar L, Shekhar V, Sharma A, Ramakrishnan L, Sharma OD, Begum A. Prevalence of Monoclonal Gammopathy of Undetermined Significance in India-A Hospital-based Study. Clin Lymphoma Myeloma Leuk. 2018 Sep;18(9):e345-e350. doi: 10.1016/j.clml.2018.06.005. Epub 2018 Jun 12. PMID: 29980412.
2. Kyle RA, Therneau TM, Rajkumar SV, et al. Prevalence of monoclonal gammopathy of undetermined significance. N Engl J Med 2006; 354:1362.
3. Smith A, Howell D, Patmore R, et al. Incidence of haematological malignancy by sub-type: a report from the Haematological Malignancy Research Network. Br J Cancer 2011; 105:1684.
4. Greenberg AJ, Rajkumar SV, Vachon CM. Familial monoclonal gammopathy of undetermined significance and multiple myeloma: epidemiology, risk factors, and biological characteristics. Blood 2012; 119:5359.
5. Landgren O, Kristinsson SY, Goldin LR, et al. Risk of plasma cell and lymphoproliferative disorders among 14621 first-degree relatives of 4458 patients with monoclonal gammopathy of undetermined significance in Sweden. Blood 2009; 114:791.
6. Kyle RA, Therneau TM, Rajkumar SV, et al. Prevalence of monoclonal gammopathy of undetermined significance. N Engl J Med 2006; 354:1362.
7. Dispenzieri A, Katzmann JA, Kyle RA, et al. Prevalence and risk of progression of light-chain monoclonal gammopathy of undetermined significance: a retrospective population-based cohort study. Lancet 2010; 375:1721.
8. Kyle RA, Larson DR, Therneau TM, et al. Long-Term Follow-up of Monoclonal Gammopathy of Undetermined Significance. N Engl J Med 2018; 378:241.
9. Kyle RA, Therneau TM, Rajkumar SV, et al. A long-term study of prognosis in monoclonal gammopathy of undetermined significance. N Engl J Med 2002; 346:564.
10. Kyle RA, Larson DR, Therneau TM, et al. Long-Term Follow-up of Monoclonal Gammopathy of Undetermined Significance. N Engl J Med 2018; 378:241.
11. Axelsson U. A 20-year follow-up study of 64 subjects with M-components. Acta Med Scand 1986; 219:519.
Introduction
Transient elastography (TE) is a commonly used ultrasound-based shear wave elastography (SWE) technique for assessing hepatic fibrosis. It is primarily used as an alternative to liver biopsy for the assessment of hepatic fibrosis and is quick, painless and non-invasive.
Principle:
Transient elastography (TE) is performed using transducer-induced vibrations at a low frequency (50 Hz) and amplitudes. Liver stiffness is evaluated by measuring the velocity of a vibration wave (also called a shear wave) generated on the skin. The transmitted shear waves propagate through the liver parenchyma. In TE, the shear waves are generated by a mechanical piston with a single-element ultrasound transducer. It is used to lightly push the skin over an intercostal space, resulting in a shear wave that travels through the liver. Measurements are then taken along the direction of the ultrasound beam.
Results are expressed in kPa and can range from 2.5 to 75 kPa
How to do?
Patient needs fasting for 4 hours and requires to lie on their back with their right arm above the head, providing access to right rib cage so that liver can be scanned. Measurements are taken from the right lobe of the liver via the 9th, 10th, or 11th intercostal space. vibrations can be felt as the device sends energy pulses to liver to gather measurements.
To improve test reliability a minimum of 10 valid readings, with at least a 60% success rate and an interquartile range of =30% of the median value, are taken with the results expressed in kilopascals (kPa).
Indications and clinical applications:
1.People who have risk factors for liver disease, such as a history of heavy alcohol intake or
presence of diabetes and/ or overweight/obesity.
2. People who have evidence of a liver condition where there is a need to work out the severity, and for baseline assessment:
� Non-alcoholic fatty liver disease
� Alcohol-related liver disease
� Abnormal liver tests of unknown cause
� Autoimmune liver disease and biliary conditions such as PBC and PSC
� Haemochromatosis
� Monitoring the liver in patients taking medication that can cause liver damage (e.g., methotrexate).
3. To estimate the existing degree of liver damage-monitor disease progression or regression via serial measurements.
4. Treatment monitoring: To assess changes in liver stiffness during antiviral therapy, monitoring treatment response.
5. Liver transplant evaluation: To assess liver fibrosis in liver transplant donor.
6. Cirrhosis diagnosis: To identify cirrhosis and assess its severity.
7. HCC screening: To evaluate liver stiffness in patients with increased risk of hepatocellular carcinoma.
8. Population screening: To identify individuals with liver fibrosis in high-risk populations.
Interpretation:
CAP Score: The amount of liver with fatty change is measured by CAP score in decibels per meter (dB/m) and corresponds to steatosis grade (S1, S2 or S3). The lower the percentage of liver with fatty change, the healthier your liver is and lower the CAP score and steatosis grade from your FibroScan. A CAP score of 5% or lower indicates a healthy liver, while a CAP score of 6% to 33% with a steatosis grade of S1 indicates a mild fatty liver. CAP scores and steatosis grades higher than that indicate moderate to severe liver fat content and more liver damage.
|
CAP value |
Grading |
Interpretation |
|
< 237 dB/m (<5%) |
S0 |
No steatosis |
|
237-259 dB/m |
S1 |
Mild steatosis |
|
259-291 dB/m (34-66%) |
S2 |
Moderate steatosis |
|
291-400 dB/m (>66%) |
S3 |
Severe steatosis |
Fibrosis Score: Based on the amount of scarring in your liver, as measured in kilopascals (kPa), we will receive a fibrosis score. A lower score indicates less liver scarring and a healthier liver. A normal result is between 2 and 6 kPa. A fibrosis score of F0 to F1 indicates no liver scarring or mild liver scarring. The highest score possible is F4, which indicates advanced liver scarring or cirrhosis. However, the LSM values differ according to the underlying etiology.
|
LSM value |
Grading |
Interpretation |
|
< 5.5 KPa |
F0 |
No fibrosis |
|
5.5-8 KPa |
F1 |
Mild fibrosis |
|
8-10 KPa |
F2 |
Moderate fibrosis |
|
11-16 KPa |
F3 |
Severe fibrosis |
|
>� 16 KPa |
F4 |
Cirrhosis |
Drawbacks/limitations:
1. Lack of anatomic orientation
2. Limited depth of penetration
3. Specific requirements for patient positioning.
4. Fluid (ascites) and adipose tissue attenuate shear wave propagation.
5. Avoided in patients with implantable pacemakers or cardioverter-defibrillator.������
Dr. Pushkar Kumarchandra Patil; ppatilpushkar@gmail.com
Dr. KNK Shetty
knkshetty@hotmail.com
A Case Report.
Srinivas Nalloor, Impana GN, Ranjitha VN, Benaganahalli Shivalingappa Sandeep, Raghavendra, Anish Behl.
Abstract
Conn�s Syndrome or Primary Aldosteronism(PA) due to aldosterone producing adrenal adenoma(APA) is the most frequent cause of hypokalemia and secondary hypertension. We are reporting a similar case in an Indian male, who presented with recurrent� lower limb weakness,� hypertension who needed admission twice for management of� same. On evaluating, laboratory reports revealed his symptoms re due to refractory severe hypokalemia, metabolic alkalosis, raised serum aldosterone levels and low plasma rennin activity. Trans Tubular Potassium Gradient (TTKG) was suggestive of ongoing renal potassium loss. CT angiography of adrenal glands during his first admission showed 8mm nodule in the right adrenal gland. CT angiography during his second admission with more severe similar complaints revealed increase in size of this nodule.
The patient was managed with serum potassium correction and surgical intervention. He underwent laparoscopic right adrenalectomy. Following the surgery, patient serum potassium normalized and he had good clinical outcome. We suggest� clinicians to consider screening for primary aldosteronism and offer surgical intervention wherever necessary in cases with refractory hypokalemia and secondary hypertension.
Introduction
Aldosterone is secreted from the medulla of the adrenal gland, raised K+ is its primary release stimulus. It is also released during hyponatremia and hypotension. In Primary Aldosteronism, excess aldosterone suppresses� renin, influx Na+ and outflux K+, causing hypertension and hypokalemia, this was first reported in 1953 by Dr Litynski[1].The subtypes that can cause primary aldosteronism is bilateral(60%) or unilateral(2%)� adrenal hyperplasia, aldosterone producing adrenal adenoma(30%) and rarely glucocorticoid responsive aldosteronism[2-3].Other subtypes include pure aldosterone producing adrenocortical carcinoma(<1%),familial hyperaldosteronism (<1%),ectopic aldosterone producing adenoma or carcinoma(<1%)[3].Primary Aldosteronism affects 1% of hypertensive population, and there is evidence showing its prevalence has increased in recent years ranging from 5% to 20% in� resistant hypertension[4].A study on prevalence of Primary Aldosteronism in primary care, a cross sectional study showed 2.6% prevalence in primary care settings[5].The prevalence of Aldosterone producing adenoma was 4.9% in comparison to bilateral adrenal hyperplasia which was 1.2% and unilateral adrenal hyperplasia which was 0.1%� as per a prospective study from Japan[6-7].It is important to identify the subtypes causing primary aldosteronism in order to plan medical or surgical line of management &� for good clinical results.
Case report
A 44year old male presented to emergency of Apollo BGS Hospital, Mysore, with complaints of sudden onset low backache, body ache and generalized weakness of three days duration. He was diagnosed to have secondary hypertension and was on treatment for recurrent hypokalemia induced skeletal muscle weakness since 2019.He was then treated with K+ correction with KCL and dual Anti-Hypertensive, Cilnidipine 10mg BD and Eplerenone 25mg BD, He recently changed Anti-Hypertensive medicine to Aldactone 25mg BD and Amlogard 5mg BD.
On examination ,he was afebrile, HR 92/min, BP was 150/100mmHg.Hand grip weakness was there on left side (he had right lower limb weakness on his previous admission).Systemic examination otherwise was unremarkable. Laboratory values showed severe hypokalemia(1.8mmol/L).Rest of the laboratory values were with in normal limits. Arterial Blood Gas analysis (ABG) showed metabolic alkalosis,2D ECHO was normal, Serum aldosterone levels previously done on OPD basis were high(34.5ng/dl) and plasma renin activity was suppressed(2.37). Serum Aldosterone level and Plasma Renin Activity (SAL/PRA) ratio was also significantly high suggestive of primary aldosteronism. The contrast CT scan of adrenal glands showed focal lesion in medial limb of right adrenal gland measuring 12 x 9 x 12 mm (APXTransverseXvertical),absolute wash out = 75%, relative washout = 44%,wash out features favored possibility of adenoma(Fig 6-8).
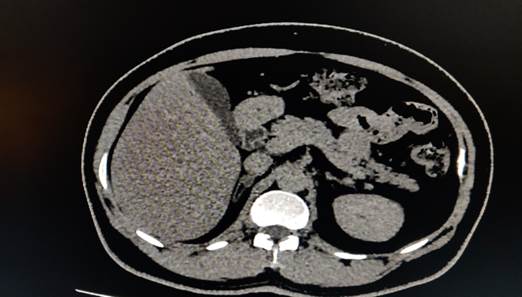
Fig 6: Plain CT axial section showing 12x8 mm sized nodule with attenuation of +28HU.

Fig 7:60 sec post contrast showing attenuation of +68HU.
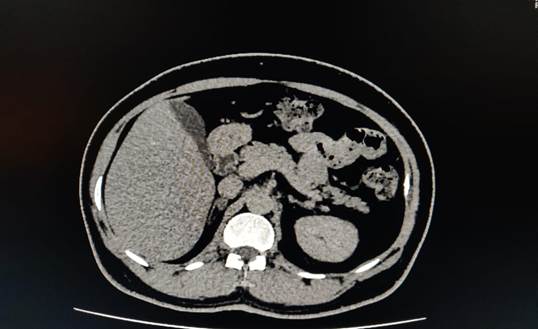
Fig 8: 15mins delayed axial CT sections showing attenuation of +35 HU. Absolute wash out ratio is 75per & relative washout ratio is 44per. Wash out feature is diagnostic of Benign Adrenal Adenoma.
Neurologist opinion was also taken to rule out any other neurological causes for limb weakness. Endocrinology opinion was taken and 24hours metanephrin test was done, it was elevated. He was treated with potassium chloride Intravenous supplementation. Once the diagnosis was confirmed, urologist opinion was taken and he underwent laparoscopic right adrenalectomy. Following surgery his serum potassium levels normalized and he improved clinically and he was discharged.
The Anatomical specimen excised was sent for histopathological examination.(Fig 9 - 15).

Fig 9: Fresh specimen.

Fig 10: Serial sections of tumor
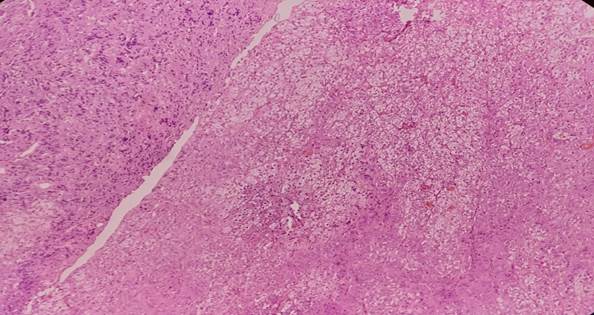
Fig 11: Demarcation between normal adrenal in left vs adenoma on right 10x.
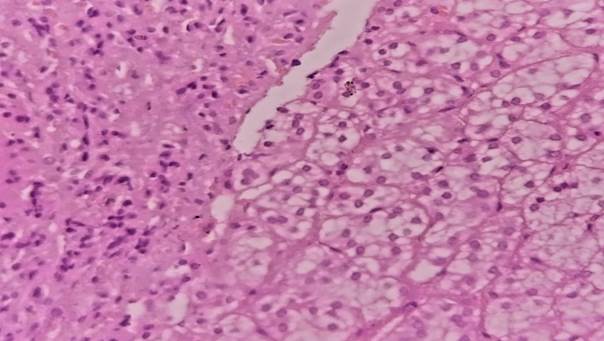
Fig 12: Demarcation between normal adrenal in left vs adenoma in right 40x
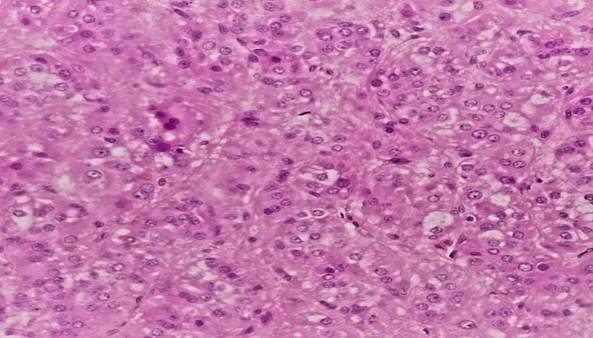
Fig 13: Adenoma per se 40x
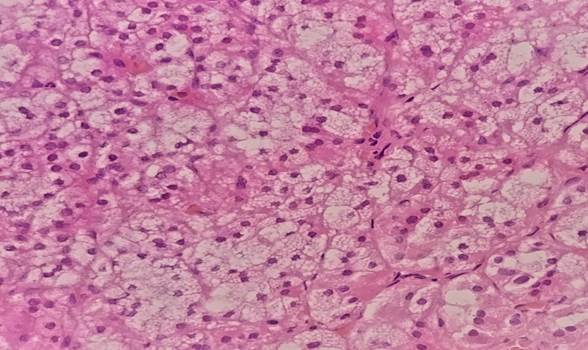
Fig 14: Areas with vacuolated cytoplasm 40x
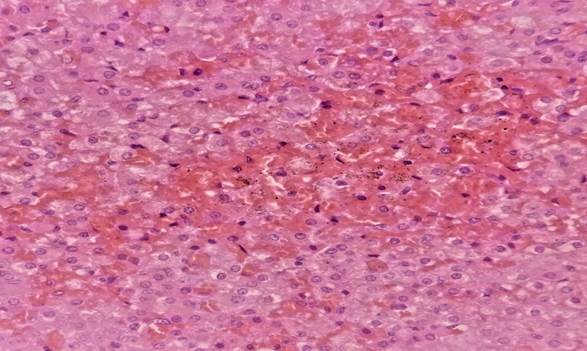
Fig 15: Areas with secondary changes of hemorrhage and hemosiderin deposition
Treatment
Medical therapy includes K+ correction with KCL, this is only symptomatic therapy. Spironolactone therapy is the treatment of choice which prevents absorption of Na+ and loss of K+. Calcium channel blockers, diuretics, ACE, or ARB Inhibitors are used for management of blood pressure. Laparoscopic Adrenalectomy is the surgical treatment of choice. Postoperatively the serum K+ and blood pressure improves significantly. Our patient� underwent right adrenalectomy. Postoperatively he was better, his laboratory and clinical parameters had improved and he� was discharged.
Outcome and follow up
The patient�s clinical parameters were normalized within 24 hours of surgery. He was discharged on second post operative day .He was on weekly follow up to begin with.
Discussion
�Adrenal adenoma causing recurrent hypokalemia and secondary hypertension is seen in most of the cases of Primary Aldosteronism(PA) reported so far. Secondary hypertension is common than hypokalemia. It can be a combination of normokalemic secondary hypertension or hypokalemic secondary hypertension[8].The screening of hypertensive patients for PA using Aldosterone to Renin Ratio has increased the prevalence of PA� from 5 to 15 fold[9].The prevalence of PA in hypertensive patients in referral centers ranges from 1� to 29.8% , contrary to primary care set up, where it ranges from 3.2% to 12.7%[10].The prevalence of hypokalemia in PA patients in referral centres ranges from 0 to 67per and in primary care centres from 0 to 37.5per[10].The prevalence of PA increases with the severity of hypertension[11,12] and the prevalence of hypokalemia increases in the same subgroups [13,14].Unilateral adrenal adenomas are also commonly seen in PA. It can occur as an isolated case or in combination with bilateral or unilateral adrenal hyperplasia[5].It is necessary to do relevant work up and definitive tests to confirm the cause of PA, the plan of management depends on these. It helps to choose surgical or medical management.
Plasma Renin Activity(PRA) and Serum Aldosterone(SA) level tests are used to diagnose PA. In presence of suppressed PRA and high serum Aldosterone levels ,CT scan of adrenal gland must be done to identify any adenoma or hyperplasia. If, CT scan doesn�t detect any adrenal mass, Adrenal Vein Sampling (AVS) must be done to diagnose unilateral or bilateral PA (lesion is lateralized to the side of sample with high level of aldosterone) and it�s the gold standard. In our case adrenal vein sampling was not done. A active adrenal adenoma on right side which showed increase in size in comparison to previous adrenal CT scan was evident. Though, sensitivity and specificity of AVS is superior to CT in detecting unilateral PA[15,16] and prevent unnecessary surgery as in case reporting of UAH and left Incidentaloma. Our patient improved following right adrenalectomy. A follow up CT scan of adrenal gland showing progressive changes correlating with the worsening clinical symptoms and lab parameters require prompt referral and surgical intervention.
Conclusion
A case of Adrenal adenoma causing hypokalemia and secondary hypertension is reported. Clinicians need to be on the lookout for this rare condition while investigating the causes for resistant hypertension & refractory hypokalemia in primary care settings.
References:
1. Kucharz EJ. Michał Lityński�a forgotten author of the first description on primary hyperaldosteronism. Pol Arch Med Wewn 2007;117:57�8.� Stewart
2. PM. Mineralocorticoid hypertension. Lancet 1999;353:1341�7. 10.1016/S0140-6736(98)06102-9 [PubMed] [CrossRef] [Google Scholar
3. Moraitis A, Stratakis C. Adrenocortical causes of hypertension. International Journal of Hypertension. 2011;2011 Article ID 624691. [PMC free article] [PubMed] [Google Scholar]
4. Riccardo Maria Fagugli * and Chiara Taglioni� Changes in the Perceived Epidemiology of Primary Hyperaldosteronism. Published online 2011 Aug 4. doi: 10.4061/2011/162804 . Available from : www.ncbi.nlm.nih.gov/pmc/articles/PMC3151507/
5. Sabine C K�yser 1, Jaap Deinum 2, Wim Jc de Grauw 1, Bianca Wm Schalk 1, Hans Jhj Bor 1, Jacques Wm Lenders 3, Tjard R Schermer 1, Marion Cj Biermans 1� . Prevalence of primary aldosteronism in primary care: a cross-sectional study . Br J Gen Pract. 2018 Feb;68(667):e114-e122. doi: 10.3399/bjgp18X694589. Epub 2018 Jan 15.
6. Omura M, Saito J, Yamaguchi K et al. . Prospective study on the prevalence of secondary hypertension among hypertensive patients visiting a general outpatient clinic in Japan. Hypertens Res 2004;27:193�202. 10.1291/hypres.27.193 [PubMed] [CrossRef] [Google Scholar] .
7. Ross EJ. Conn's syndrome due to adrenal hyperplasia with hypertrophy of zona glomerulosa, relieved by unilateral adrenalectomy. Am J Med 1965;39:994�1002. 10.1016/0002-9343(65)90122-1 [PubMed] [CrossRef] [Google Scholar] .
8. Mulatero P, Stowasser M, Loh K et al.. Increased diagnosis of primary aldosteronism, including surgically correctable forms, in centers from five continents. J Hypertens 2004;22 (Suppl 2):S182 10.1097/00004872-200406002-00629 [PubMed] [CrossRef] [Google Scholar.
9. �Mulatero P, Stowasser M, Loh KC, Fardella CE, Gordon RD, Mosso L, Gomez-Sanchez CE, Veglio F, Young Increased diagnosis of primary aldosteronism, including surgically correctable forms, in centers from five continents.J Clin Endocrinol Metab. 2004; 89:1045�1050. doi: 10.1210/jc.2003-031337CrossrefMedlineGoogle Scholar.
10. K�yser SC, Dekkers T, Groenewoud HJ, van der Wilt GJ, Carel Bakx J, van der Wel MC, Hermus AR, Lenders JW, Deinum J. Study heterogeneity and estimation of prevalence of primary aldosteronism: a systematic review and meta-regression analysis.J Clin Endocrinol Metab. 2016; 101:2826�2835. doi: 10.1210/jc.2016-1472CrossrefMedlineGoogle Scholar
11. Rossi GP, Bernini G, Caliumi C, Desideri G, Fabris B, Ferri C, Ganzaroli C, Giacchetti G, Letizia C, Maccario M, et al.; PAPY Study Investigators. A prospective study of the prevalence of primary aldosteronism in 1,125 hypertensive patients Am Coll Cardiol. 2006; 48:2293�2300. doi: 10.1016/j.jacc.2006.07.059CrossrefMedlineGoogle Scholar
12. Monticone S, Burrello J, Tizzani D, Bertello C, Viola A, Buffolo F, Gabetti L, Mengozzi G, Williams TA, Rabbia F, et al. Prevalence and clinical manifestations of primary aldosteronism encountered in primary care practice. J Am Coll Cardiol. 2017; 69:1811�1820. doi: 10.1016/j.jacc.2017.01.052CrossrefMedlineGoogle Scholar
13. Calhoun DA, Nishizaka MK, Zaman MA, Thakkar RB, Weissmann P. Hyperaldosteronism among black and white subjects with resistant hypertension. Hypertension. 2002; 40:892�896. doi: 10.1161/01.hyp.0000040261.30455.b6LinkGoogle Scholar
14. Douma S, Petidis K, Doumas M, Papaefthimiou P, Triantafyllou A, Kartali N, Papadopoulos N, Vogiatzis K, Zamboulis C. Prevalence of primary hyperaldosteronism in resistant hypertension: a retrospective observational study. Lancet. 2008; 371:1921�1926. doi: 10.1016/S0140-6736(08)60834-XCrossrefMedlineGoogle Scholar
15. Nwariaku F. Primary Hyperaldosteronism: effect of adrenal vein sampling on surgical outcome. Arch Surg 2006;141:497�502; discussion 502-3 10.1001/archsurg.141.5.497 [PubMed] [CrossRef] [Google Scholar]
16. Daunt N. Adrenal vein sampling: how to make it quick, easy, and successful1. RadioGraphics 2005;25(Suppl 1):S143�58. 10.1148/rg.25si055514 [PubMed] [CrossRef] [Google Scholar]
Fig 16: The patient in the OPD � A representative image
Mr Santhosh, a 34-year-old gentleman has had 4 episodes of left ureteric colic from December 2022 to October 2023. His ultrasound report showed multiple small stones in the substance of both kidneys. As the episodes were too frequent and going by the experience it was decided to do a serum calcium and a parathormone level. This was done on10/10/23. Calcium was 11 and PTH was 217. A parathyroid adenoma was suspected, and he was subjected to a parathyroid scintiscan on 12/10/23 which and subsequent biopsy confirmed the diagnosis. He was subsequently operated upon on20 /10/23.

Fig 17: Parathyroid adenoma (Courtesy: Radiopaedia)
Ultrasound� done on9/12/23 showed a right kidney calculus in the mid pole and a 3 to 4 mm calculus in the mid and in lower pole of the left kidney.
A follow up Ultrasound done on 24/8/24 showed no stone in the right kidney and no stone in the mid pole of the left kidney. However, the stone in the lower pole was till there but had not increased in size.
In the past 9 months he has not had any episodes of ureteric colic and no new stone formation and the old ones seem to be getting absorbed or have passed down without causing any symptoms
Calcium oxalate/phosphate stones form up to 80% of urinary stones. 9% are urate stones. Any person who gets repeated episodes of urinary colic and presence of multiple stones needs to be investigated for the presence of a parathyroid adenoma. Patients with hypermetabolic states and high cell turn over like in malignancies [ Multiple myeloma Lymphoma], Thyrotoxicosis, Sarcoidosis, Osteoporosis, AV shunts and high intake of vit D, may also present with� ureteric colic due to calcium oxalate stones,
I draw the reader�s attention to another case report of parathyroid adenoma with multi-organ involvement, published in the newsletter of May 2017/ volume/1/Issue 1.
For further information and operative details please go to [National Medical Journal of India 2007/Jan-Feb.] Dr.S.P Somasekar et al
B.C. Rao
Many illnesses are directly linked to brain activity. This happened just a week ago with a patient of mine.

Fig 18: A representative image of brain activity
This patient who is on blood pressure medication records her pressure at home and mostly it is within the normal range. But whenever I take her pressure, it is way above normal. I tried consoling her that this is a well-known phenomenon and we have even coined this as white coat hypertension.
She was not convinced and said, �I am a calm person, I have known you for many years and there is nothing here to get excited about [this is true!], your measuring instrument is showing the wrong reading.�
I have learnt not to argue with some patients and this is one of them. I said, �right then, you bring your instrument tomorrow and we will check the pressure with both the machines and see which one shows the correct reading�
She came next day. I do not know which one of us was more anxious! She took her blood pressure which showed even higher reading than the previous day! Then I took her pressure using her instrument first and then mine. The readings were less than hers!
She was convinced but wanted to know why the reading done by me was lower than hers.
�The excitement was already over when I took the reading, therefore the figures were lower� I said.
I hope she will have more faith in me and my equipment henceforth.
B C Rao
