President's Letter
Season's Greetings from AFPI Karnataka Chapter! As we approach the end of the year, I am delighted to share the accomplishments of the AFPI Karnataka chapter over the past quarter. Our new committee has hit the ground running, and we have had a fantastic three months.
Recent Initiatives:
- Led by Dr. Madhumita, our first physical meeting focused on infectious diseases, including tuberculosis, HIV, hepatitis B, C, and pyrexia of unknown origin.
- Landmark Certification Program: We launched a pioneering certification program, offering training in specialized areas like hematology. This program has garnered significant interest, with over 130 participants enrolled in the hematology course. This is the first of its kind in the history of AFPI in collaboration with international bodies like the international hematology consortium.
- Webinar on Medico-Legal aspects: Our webinar on medico-legal aspects in daily practice received an overwhelming response from participants, prompting us to plan a follow-up series.
- Conference Preparations: We are actively preparing for our upcoming international conference [WONCA], scheduled for April 4-6 at the Sheraton Grand. With over 300 registrations already received, we encourage all AFPI members to participate and share their knowledge.
Community Outreach:
- Breast cancer awareness talks
- Health talks on adult vaccination and de-addiction
- Public forums, bank employee events, and radio shows
As the president of the AFPI Karnataka chapter, I am proud of our accomplishments and grateful for the enthusiasm and dedication of our members. I wish you all a joyous festive season and look forward to a productive, healthy, and happy new year.
Stay Connected: For updates on our activities, conferences, and certification programs, please visit our website or follow us on social media.
Regards,
Dr. Sowmya B Ramesh
President, AFPI Karnataka
drsowvivek@gmail.com
Secretary's Note
Warm greetings to all of you! As we embark on another promising year together, I take this opportunity to thank each one of you for your active participation and support in the various events and initiatives organized by the Academy of Family Physicians, Karnataka Chapter. Your enthusiastic involvement, particularly in large numbers, has been the cornerstone of our success, enabling us to further our mission of advancing the family medicine specialty.
The strength of any organization lies in the collective efforts of its members. I urge all of you to continue this momentum by actively participating in our academic activities, workshops, and conferences. Together, we can elevate the standards of family medicine and make a meaningful impact on healthcare in our community.
I also encourage you to bring your friends and colleagues into our fold, increasing our membership and expanding our reach. A larger, more diverse membership will help us pool ideas, share experiences, and amplify our voice as advocates of family medicine.
As members of this esteemed association, I invite you to take up more responsibilities, contribute your expertise, and play an active role in shaping the future of our profession. Whether it is through leadership roles, mentorship, or volunteering, your contributions can strengthen our association and advance the family medicine specialty.
Additionally, your ideas and feedback are invaluable to us. We welcome your suggestions to improve our initiatives, enhance our events, and strengthen our association further. Please feel free to share your thoughts and recommendations – every voice matters in our collective journey toward growth and excellence.
Let us continue to work together to foster a culture of excellence, learning, and collaboration within our association.
With warm regards,
Dr. Hemavathi D
Hon Gen Secretary, AFPIKA
Editor's Note
A major conference is coming up in the city [WONCA South Asia Region Family Medicine] from 4/4/25 to 6/4/25. It is necessary that all family physicians participate in this conference because it is going to focus on the future of family medicine and all aspects from training to empowerment and how best to lobby and get the government to strengthen the discipline of family medicine and thus improve health care delivery. It will also discuss the ways and means of getting more young doctors to take up this specialty as a career option.
This first issue of the new year carries many features of interest. A leading article on Hyperthyroidism, a critical appraisal of asymptomatic stones, and educative and interesting case stories and updates. I am happy that the new office bearers are taking a lot of interest in the academic and social activities of the association.
B.C Rao
badakere.rao@gmail.com
Chief Editor
AFPI News
AFPI Karnataka’s new executive committee consists of a team of young passionate and wise experienced members.
- Dr. Sowmya B Ramesh, President
- Dr. Harshapriya Jyothinagar, Vice President
- Dr. Hemavathi Dasappa, General Secretary
- Dr. Supritha K M, Treasurer
- Dr. Madhumitha R, Member
- Dr. Ravi Kulkarni, Member
- Dr. Impana G N, Member
- Dr. Amrutha J H, Member
Events:
- Spice Route India Movement organized an online webinar on September 19th on the topic “Pursuing our Hobbies alongside our work” to reinforce the importance of work-life balance and how important it is not to let go of one’s hobbies to maintain a healthy living.
- On 25th September, Dr. Sowmya, President of the AFPI Karnataka chapter, spread awareness on breast cancer by giving a talk at Nalpad Academy International School.
- FMPC 2024 was organized in Rishikesh between the 28th to 29th of September with knowledge sharing on various topics. The event was dynamic with the latest updates.
- On 21st October, Dr. Sowmya delivered a health talk on the importance of adult vaccination to Canara Bank employees.
- On 25th October, Dr. Madhumitha emphasized the importance of adult vaccination to the public both online and offline in her clinic.
- The Rajyotsava celebration proved that the doctors of AFPI are very vibrant, with Dr. Mohan proving his talent as a singer by singing Kannada songs and Dr. Shaini performing a beautiful classical dance at their respective communities.
- On 6th November, Dr. Madhumitha enlightened the members of Rotary Prime by giving a talk on “Importance of health and wellness.”
- On 8th December, the first offline CME with KMC points was conducted by the new EC committee on infectious diseases with a positive number in the audience.
- AFPI Karnataka chapter organized the National API webinar on 11th December to create awareness on “Medicolegal issues in Primary care.”
- The Spice Route Karnataka conducted two academic sessions on 20th November and 18th December with case presentations, which were beneficial for PG students PAN India.
- On 22nd December, Dr. Krithika conducted a mass adult influenza campaign with Zydus and vaccinated more than 100 elderly.
- On 23rd December, Dr. Sowmya reiterated the importance of adult vaccination on Akashvani with the general public as the audience.
- On 25th December, Dr. Madhumitha conducted a health check-up at Jnanahdeep Trust Orphanage for children aged 5–18 years and gave a health talk on “Importance of cleanliness and simple measures to prevent infections.”






Featured Articles
Approach to Hyperthyroidism
Case 1
History
Tremors of the hand
Increased frequency of passing stools
Feverish feeling on most of the days
Weight loss of 20 kg in 1 year
Increased appetite
Swelling in front of the neck for 2 months
On examination:
Fine tremors
Pulse: 138/min
BP: 148/87mmhg
Uniformly enlarged thyroid gland

Figure 7 Clinical features
Case 2
History
A 55-year-old woman
2-year history of neck swelling that has gradually increased in size.
Over the past 6 months, she has experienced unintended weight loss of 7 kg despite good appetite.
Recurrent episodes of palpitations, heat intolerance, excessive sweating, and tremors.
Figure 8 Thyroid swelling
On examination:
Pulse:110/min , BP:130/80 mmHg
Enlarged thyroid, nodular and prominent on left side.
Case 3
History
A 38-year-old woman presents to the outpatient clinic with a 3-week history of anterior neck pain.
Figure 9
She reports feeling feverish, fatigued, and experiencing generalized body aches during this time. She also mentions palpitations, sweating, and weight loss of 4 kg over the last month. The symptoms started after a recent upper respiratory tract infection. She denies any difficulty swallowing, hoarseness, or family history of thyroid disease.
On examination
Temp- 38.2°C
Pulse-108 beats per minute
BP-120/80 mmHg
The thyroid gland is tender on palpation, especially over the right lobe, and is mildly enlarged but without discrete nodules.
There is no cervical lymphadenopathy
Systemic examination reveals mild tremors of the hands and warm, moist skin.
In these cases, diagnosis of hyperthyroidism is obvious. Prevalence of hyperthyroidism in general practice is not so common and identifying hyperthyroidism is not challenging. The challenge is prescribing the appropriate investigation, identifying the aetiology of the hyperthyroidism, and arriving at the most appropriate treatment plan.
In this article, we will try to simplify the choice of investigation to identify the aetiology and prescribe the appropriate treatment plan. And the contents of this article are derived from the 2018 European thyroid society guidelines and 2016 American thyroid association guidelines.
Aetiology of Hyperthyroidism
The three most common aetiologies of hyperthyroidism include:
1. Graves’ disease (GD)
2. Toxic multinodular goitre (TMNG)
3. Toxic adenoma (TA)
Other less common aetiologies of hyperthyroidism:
1. Iodine-induced hyperthyroidism
2. TSH (thyroid stimulating hormone)-secreting pituitary adenomas
3. Conditions associated with high human chorionic gonadotrophin levels: choriocarcinomas and hydatiform moles in females and germ cell tumours in males.
4. Ectopic thyroid in struma ovarii (excess thyroid hormone production from ovarian teratomas)
5. Extensive metastasis from functionally differentiated thyroid carcinoma (follicular or papillary)
6. Drug-induced thyroiditis: Amiodarone, lithium, tyrosine kinase inhibitors, interferon-alpha, immune checkpoint inhibitor therapy
7. Other thyroiditis: Hashitoxicosis, painless thyroiditis, painful subacute thyroiditis, suppurative thyroiditis, and Riedel thyroiditis
8. Factitious thyroiditis (due to excess exogenous thyroid hormone: intentional or unintentional use)
Asymptomatic Gallstones
Asymptomatic Cholelithiasis: Should we offer surgery?
Case scenario An overweight middle-aged lady reports with an ultrasound abdomen that incidentally reveals calculi in the gallbladder. There is no pain nor tenderness nor jaundice. The clinical impression is asymptomatic cholelithiasis. Should the Family Practitioner advise surgery or not?
Featured Articles
Approach to Hyperthyroidism
Case 1
History
Tremors of the hand
Increased frequency of passing stools
Feverish feeling on most of the days
Weight loss of 20 kg in 1 year
Increased appetite
Swelling in front of the neck for 2 months
On examination:
Fine tremors
Pulse: 138/min
BP: 148/87mmhg
Uniformly enlarged thyroid gland
Figure 7 Clinical features
Case 2
History
A 55-year-old woman
2-year history of neck swelling that has gradually increased in size.
Over the past 6 months, she has experienced unintended weight loss of 7 kg despite good appetite.
Recurrent episodes of palpitations, heat intolerance, excessive sweating, and tremors.

Figure 8 Thyroid swelling
On examination:
Pulse:110/min , BP:130/80 mmHg
Enlarged thyroid, nodular and prominent on left side.
Case 3
History
A 38-year-old woman presents to the outpatient clinic with a 3-week history of anterior neck pain.

Figure 9
She reports feeling feverish, fatigued, and experiencing generalized body aches during this time. She also mentions palpitations, sweating, and weight loss of 4 kg over the last month. The symptoms started after a recent upper respiratory tract infection. She denies any difficulty swallowing, hoarseness, or family history of thyroid disease.
On examination
Temp- 38.2°C
Pulse-108 beats per minute
BP-120/80 mmHg
The thyroid gland is tender on palpation, especially over the right lobe, and is mildly enlarged but without discrete nodules.
There is no cervical lymphadenopathy
Systemic examination reveals mild tremors of the hands and warm, moist skin.
In these cases, diagnosis of hyperthyroidism is obvious. Prevalence of hyperthyroidism in general practice is not so common and identifying hyperthyroidism is not challenging. The challenge is prescribing the appropriate investigation, identifying the aetiology of the hyperthyroidism, and arriving at the most appropriate treatment plan.
In this article, we will try to simplify the choice of investigation to identify the aetiology and prescribe the appropriate treatment plan. And the contents of this article are derived from the 2018 European thyroid society guidelines and 2016 American thyroid association guidelines.
Aetiology of Hyperthyroidism
The three most common aetiologies of hyperthyroidism include:
1. Graves’ disease (GD)
2. Toxic multinodular goitre (TMNG)
3. Toxic adenoma (TA)
Other less common aetiologies of hyperthyroidism:
1. Iodine-induced hyperthyroidism
2. TSH (thyroid stimulating hormone)-secreting pituitary adenomas
3. Conditions associated with high human chorionic gonadotrophin levels: choriocarcinomas and hydatiform moles in females and germ cell tumours in males.
4. Ectopic thyroid in struma ovarii (excess thyroid hormone production from ovarian teratomas)
5. Extensive metastasis from functionally differentiated thyroid carcinoma (follicular or papillary)
6. Drug-induced thyroiditis: Amiodarone, lithium, tyrosine kinase inhibitors, interferon-alpha, immune checkpoint inhibitor therapy
7. Other thyroiditis: Hashitoxicosis, painless thyroiditis, painful subacute thyroiditis, suppurative thyroiditis, and Riedel thyroiditis
8. Factitious thyroiditis (due to excess exogenous thyroid hormone: intentional or unintentional use)
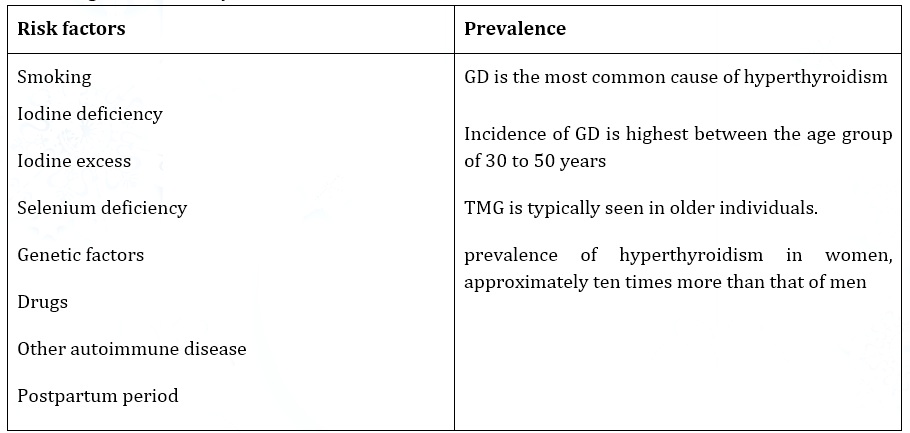
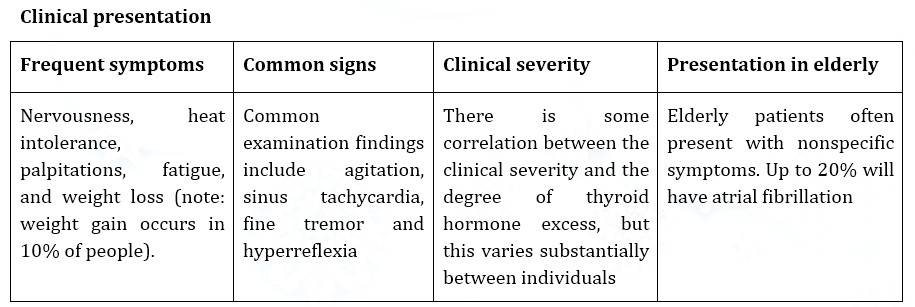
Figure 10 Investigations for the cause of thyrotoxicosis
Investigation
The aetiology of thyrotoxicosis should be determined. If the diagnosis is not apparent based on the clinical presentation and initial biochemical evaluation, diagnostic testing is indicated and can include, depending on available expertise and resources, measurement of TRAb, determination of the radioactive iodine uptake (RAIU), or measurement of thyroidal blood flow on ultrasonography.
In a patient with a symmetrically enlarged thyroid, recent onset of orbitopathy, and moderate to severe hyperthyroidism, the diagnosis of GD is likely and further evaluation of hyperthyroidism causation is unnecessary. In a thyrotoxic patient with a nonnodular thyroid and no definite orbitopathy, measurement of TRAb or RAIU can be used to distinguish GD from other aetiologies. A 123I or 99mTc pertechnetate scan should be obtained when the clinical presentation suggests a TA or TMNG.
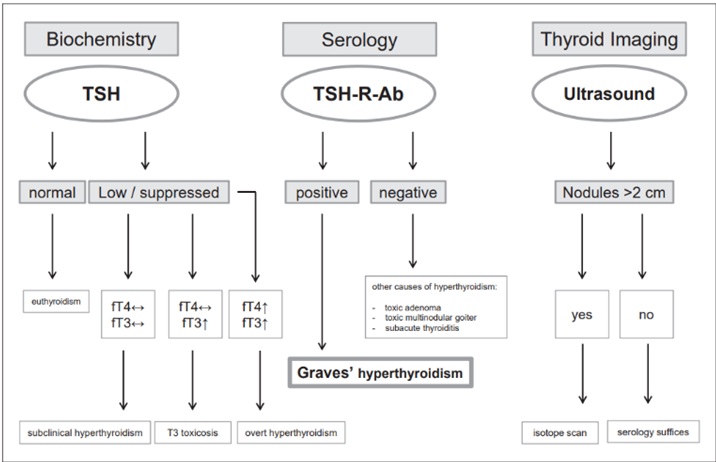
Figure 11 Approach to suspected GD-2018 European thyroid association guidelines
What do you think is the diagnosis of cases described above?
Case 1 is most probably Graves’ disease as there is severe symptoms of thyrotoxicosis, uniformly enlarged thyroid gland and orbitopathy.
Case 2 is most probably toxic multinodular goitre as there are symptoms of severe thyrotoxicosis, nodular goitre, and absence of orbitopathy.
Case 3 is most probably thyroiditis as there is short history of mild symptoms of thyrotoxicosis following an episode of URTI with neck pain and tender thyroid.
What are the investigation choices for the above cases?
Case 1: Since GD is suspected, TSH, Free T4, T3, and TSH-R-Ab could be most appropriate.
Case 2: Since toxic multinodular adenoma is suspected, TSH, Free T4, T3, and Radionuclide thyroid scan.
Case 3: Since thyroiditis is suspected, TSH, Free T4, T3, and TSH-R-Ab or Radionuclide thyroid to differentiate with GD.
Treatment of GD (Graves’ disease) (Case 1)
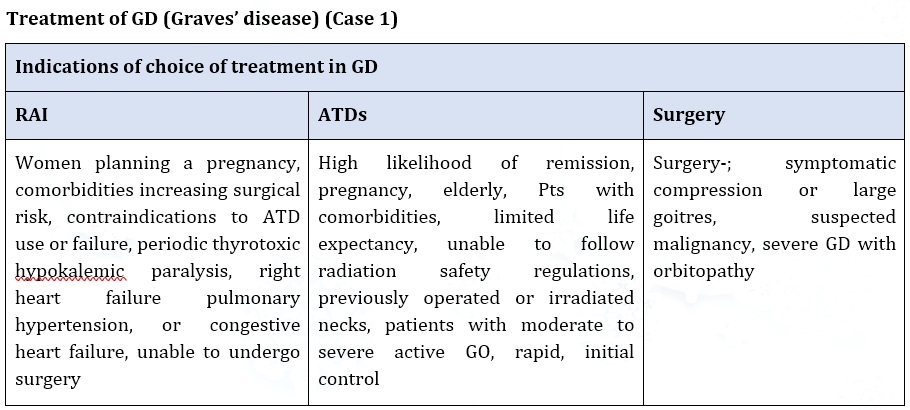
Recommendations:
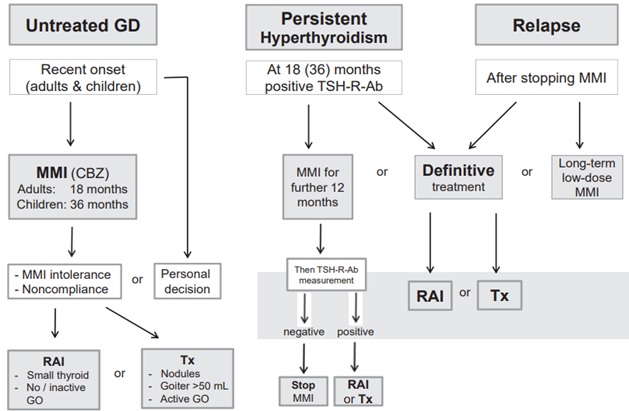
1. Patients with newly diagnosed Graves’ hyperthyroidism should be treated with ATD. RAI therapy or thyroidectomy may be considered in patients who prefer this approach.
2. MMI (CBZ) should be used in every non-pregnant patient who chooses ATD therapy for Graves’ hyperthyroidism.
3. MMI is administered for 12–18 months then discontinued if the TSH and TSH-R-Ab levels are normal.
4. Measurement of TSH-R-Ab levels prior to stopping ATD therapy is recommended, as it aids in predicting which patients can be weaned from the medication, with normal levels indicating a greater chance of remission.
. Patients with persistently high TSH-R-Ab at 12–18 months can continue MMI therapy, repeating the TSH-R-Ab measurement after anadditional 12 months, or opt for RAI or thyroidectomy.
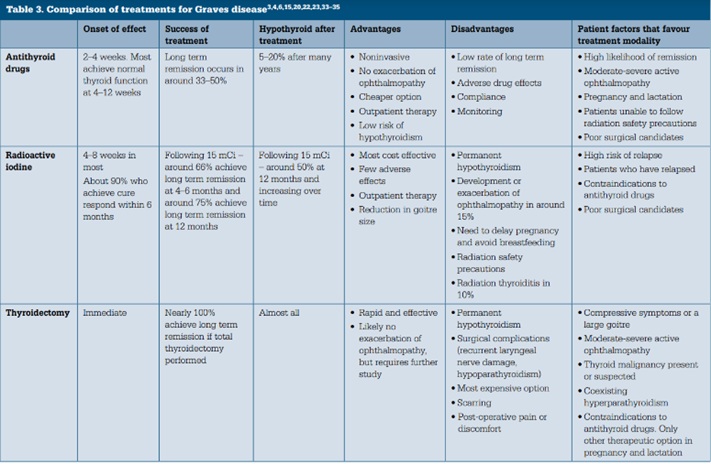
Table 3 Indications of choice of treatment in GD
MMI, methimazole; CBZ, carbimazole; GO, Graves’ orbitopathy; RAI, radioactive iodine; Tx, total thyroidectomy
Antithyroid drugs in GD
The initial dose of MMI is usually 10–30 mg once daily depending on the severity of hyperthyroidism (CBZ 15–40 mg/day
The starting dose of ATD can be gradually reduced (titration regimen) as thyrotoxicosis improves
Thyroid function tests are reviewed 3–4 weeks after starting treatment, and the dose is titrated based on free T4 and free T3 levels.
A substantial proportion of patients reach euthyroid within 3–4 weeks of treatment
TSH levels often remain suppressed for several months and therefore do not provide a sensitive index of early treatment response
The usual daily maintenance doses of ATD in the titration regimen are 2.5–10 mg of MMI and 50–100 mg of PTU.
RAI in GD
Verbal as well as written information on all aspects of efficacy and potential side-effects of RAI therapy should be provided.
If ATD are used before RAI therapy, they should be paused around 1 week before and after therapy in order not to decrease the efficacy of RAI therapy.
Conception should be postponed until at least 6 months after RAI in both males and females
Follow-up within the first 1–2 months after RAI therapy for GD should include an assessment of free T4, total T3, and TSH
Biochemical monitoring should be continued at 4- to 6-week intervals for 6 months, or until the patient becomes hypothyroid and is stable on thyroid hormone replacement
Most patients respond to RAI therapy with a normalization of thyroid function tests and improvement of clinical symptoms within 4–8 weeks
Hypothyroidism may occur from 4 weeks on, with 40% of patients being hypothyroid by 8 weeks and >80% by 16 weeks
Treatment of Graves’ disease in special situation
GD with orbitopathy
In patients with GO, hyperthyroidism should be promptly controlled by ATD, and euthyroidism stably maintained.
Patients treated with RAI should receive steroid prophylaxis if mild and active GO preexists or there are risk factors for RAI-associated GO occurrence or progression.
In patients with moderate-to-severe and active GO, treatment of GO should be the priority. Euthyroidism should be promptly restored with ATD and stably maintained.
Patients with sight-threatening GO should be treated with ATD.
Treatment for hyperthyroidism in patients with inactive GO can be selected in
GD in pregnancy
All patients with a history of autoimmune thyroid disease should have their TSH-R-Ab serum levels measured at the first presentation of pregnancy, if they are elevated, again at 18–22 weeks of gestation
If the maternal TSH-R-Ab concentration remains high (>3 times the cut-off), monitoring of the fetus for thyroid dysfunction throughout pregnancy is recommended.
During pregnancy the lowest possible dose of ATD should be given and the block-and-replace ATD regimen is discouraged.
Maternal FT4 (TT4) and TSH should be measured every 2 weeks after the initiation of therapy, and every 4 weeks after achieving the target value.
A change from PTU to MMI should be considered if ATD are required after 16 weeks gestation
In women on a low dose of MMI (<5–10 mg/day) or PTU (<50–100 mg/day), ATD may be stopped during gestation prior to weeks 6–10.
GD in elderly
Older patients who have had atrial fibrillation, cardiac failure, or cardiac ischemic symptoms precipitated by hyperthyroidism should undergo definitive therapy, usually RAI.
Long-term MMI (CBZ) should be considered as a satisfactory treatment for older individuals with mild GD.
GD in children
PTU should be avoided in children and adolescents.
Long-term MMI (CBZ) should be the mainstay of treatment in children with GD.
Thyroidectomy is the primary definitive therapy in childhood, but in post pubertal children RAI can be considered.
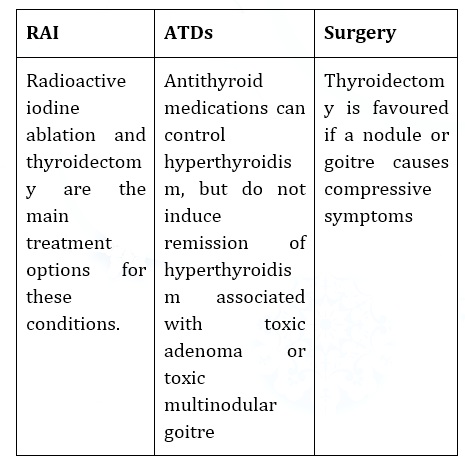
Figure 14 Treatment of toxic multinodular adenoma / toxic adenoma (case 2)
Treatment of Subacute thyroiditis (Case 3)
• Painless thyroiditis and subacute thyroiditis are self-limiting conditions that usually resolve spontaneously within six months.
• There is no role for antithyroid medications or radioactive iodine ablation in the treatment of thyroiditis.
• Beta-blockers may be used if needed to control adrenergic symptoms.
• Pain associated with subacute thyroiditis may be relieved with a nonsteroidal anti-inflammatory drug.
Adverse effects of management
Antithyroid drugs or Thioamides are associated with rare but serious adverse effects of agranulocytosis, hepatotoxicity, and vasculitis. Hepatotoxicity is more common with the use of propylthiouracil (2.7%) than methimazole (0.4%). Hepatotoxicity due to methimazole is more likely to be cholestatic, while hepatotoxicity due to PTU is more likely to be hepatocellular. Haematological complications have an incidence of 0.1-0.15% with the use of PTU or methimazole. Of these patients, 89% had agranulocytosis, and 11% had pancytopenia or aplastic anaemia. Patients taking PTU and rarely methimazole can develop p-ANCA (anti-neutrophil cytoplasmic antibody) positive small vessel vasculitis. Up to 40% of those taking PTU can develop c-ANCA positivity, but very few develop vasculitis. These medications are also associated with the development of drug-induced lupus. Few cases of hypoglycaemia secondary to autoimmune insulin syndrome have been reported using methimazole.
If patients develop an acute febrile illness with symptoms of pharyngitis, they should get blood work done to check complete blood cell counts along with differentials to rule out the development of agranulocytosis. Liver function tests should be assessed in patients who develop a pruritic rash, abdominal pain or bloating, anorexia, nausea, vomiting, fatigue, jaundice, light-colored stool, or dark urine.
The most common complications following total or near-total thyroidectomy include hypocalcaemia due to hypoparathyroidism in less than 2% of cases (can be transient or permanent), recurrent or superior laryngeal nerve paralysis in less than 2% of cases (can be temporary or permanent), haemorrhage, and complications related to anaesthesia.
Asymptomatic Cholelithiasis: Should we offer surgery?
Case scenario
An overweight middle-aged lady reports with an ultrasound abdomen that incidentally reveals calculi in the gallbladder. There is no pain nor tenderness nor jaundice. The clinical impression is asymptomatic cholelithiasis. Should the Family Practitioner advise surgery or not?
Evidence-Based Medicine
Currently, medical decision making has moved towards Evidence Based Medicine EBM that is commonly misunderstood as being purely dependent on scientific published evidence. Yes, it remains a key component, but EBM as illustrated in Figure A depends not only on scientific literature (i.e. Evidence), but on the clinician’s experience and patient’s context (values, beliefs, socio-economic-cultural background).
Figure A: Components of Evidence Based Medicine
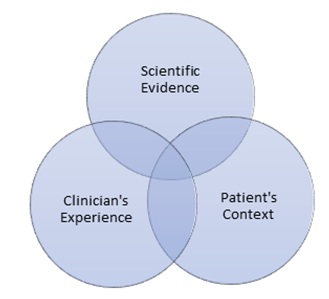
Figure 16 Components of evidence-based medicine
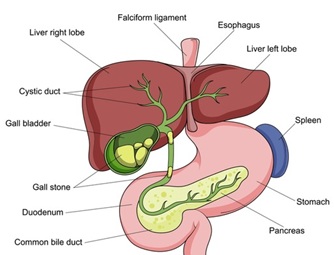
Cholelithiasis “Gall Stones”
The presence of calculi in the gallbladder is termed cholelithiasis. Calculi usually develop secondary to supersaturation and concentration of bile, crystal nucleation and gall bladder dysmotility. For cholesterol calculi, the triangle of solubility includes cholesterol, lecithin and bile salts. Disturbances in these proportions lead to collection of insoluble cholesterol forming sludge that in term precedes calculi. The predominant solute that precipitates into calculi determines the classification into Cholesterol (common at 80-90%) or Pigment calculi.
Clinical features
Cholelithiasis is asymptomatic in approximately 80% of adults. This is usually an incidental finding on an ultrasound abdomen performed for unrelated symptoms. Other patients present with symptoms of biliary colic, acute cholecystitis, chronic cholecystitis, gallbladder mucoceles, and empyema of the gall bladder. Inflammation secondary to infection is a usual process in those symptomatic. Symptoms may include fever, nausea, vomiting, pain in the upper right abdomen, distention, jaundice and a palpable mass. Features of dyspepsia makes it difficult to attribute it to cholelithiasis.
Risk factors
Traditionally one remembers risk factors for cholelithiasis and its complications as the 4 ‘Fs’ (Female, Forty, Fat, Fertile). A fifth factor may be less relevant for us being a Fair race (Caucasian). These risk factors may be classified as modifiable or nonmodifiable factors as tabulated below (Table 4):
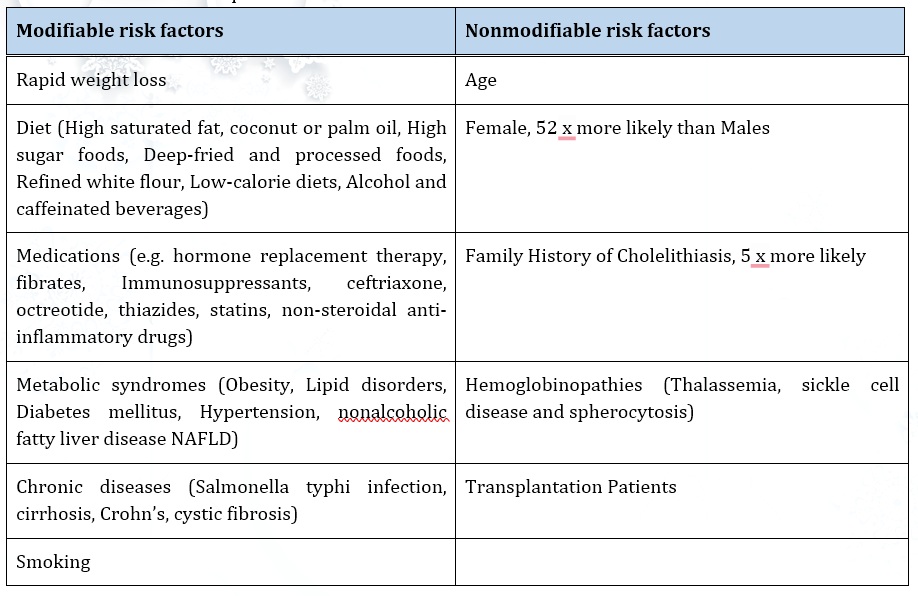
Table 4 Risk factors for cholelithiasis
Parameters for a medical decision-making process
To determine the next steps in management when cholelithiasis is detected and the patient is asymptomatic requires one to weigh the pro and con of the treatment alternatives. Therapeutic options include conservative ‘wait and watch’ versus interventional surgical cholecystectomy. To present a patient with options enabling informed consent one needs to understand and explain the following factors:
Likelihood of progress from asymptomatic to symptomatic/complication
Likelihood of complications of surgery/anaesthesia
Progress from asymptomatic to symptomatic/complication
It is traditionally estimated that 1-4% (literature varies from 0.1% to 7.3%) of asymptomatic cholelithiasis patients every year progress to develop symptoms. Over a period, progression from asymptomatic to symptomatic gallstone disease ranged from 11.7% to 23.7% (up to 30%) over 9-20 years follow up period. The cumulative incidence of developing complications for asymptomatic gallstone patients has been estimated at about 3%-8% over the same period. The lifetime risk of progressing to symptomatic disease is said to be 20% compared to the low morbidity associated with modern laparoscopic with rates increasing to 40% especially in females. Symptomatic cholelithiasis presents with uncomplicated symptoms or biliary colic in 70% and 30% may have severe conditions like sepsis or pancreatitis. Hence, symptomatic cholelithiasis mandates surgery.
Complications post-surgery/anaesthesia
The determining parameter may be the proportion or probability of complications if one intervenes secondary to the underlying condition or surgery or anaesthesia. Or if one chooses to go conservative, the proportion or probability of the asymptomatic patient progressing to develop symptoms or complications of the underlying condition that is already explained above. Risks directly related to the intervention (Surgery and Anaesthesiology) and comorbidities likely to complicate issues also need to be considered. Most literature recommends that surgery should not be routinely offered to asymptomatic cholelithiasis with only reassurance and watchful waiting being required. This is primarily in view of inherent risks of surgery and anesthesia that includes potential vascular and bowel injuries, retained stone, bile leak, bile duct Injury and post cholecystectomy syndrome. However, with no randomized trials comparing cholecystectomy versus no cholecystectomy in patients with asymptomatic gallstones there exists no evidence to assess surgical treatment in asymptomatic gallstones. Advances in anesthesiology and surgical techniques like laparoscopy and robotics are changing the risks. Laparoscopic cholecystectomy has a lower rate of complications than open surgery though bile duct injury is a more common complication. Hospital stays are shorter and post operation patient comfort better. Lower mortality and cardiac morbidity are found in laparoscopy versus open surgery. So, with this information, do we recommend surgical interventions or remain conservative in dealing with a patient with asymptomatic cholelithiasis?
Decision Making Process
Given the information provided, alternatives exist even for asymptomatic cholecystectomy. The inclusion of the patient in the medical decision-making process challenges the blanket rule of not routinely advising a prophylactic cholecystectomy given existing reduced risks due to advances and long-term risk of symptoms and complications.
A Markov chain model is a random probability distribution or pattern model that is satisfied when current state of the process is enough to predict the future state of the process and the prediction should be as good as making prediction by knowing their history. Lee BJH et al used a Markov Assumption Model for asymptomatic gallstones that revealed interesting insights making a case for patient decisions rather than a blanket rule against intervention for asymptomatic cholelithiasis. They suggested that if conservative management of uncomplicated asymptomatic cholelithiasis adults, one would expect 40% progressing to symptoms of which 30% would end up with serious pancreatitis and sepsis. This process prediction balanced against all asymptomatic being operated that would result in 99.5% recovering with no complications. Given the approximately
Present Indian guidelines from the Indian Council of Medical Research ICMR and Ministry of Health and Family Welfare, Government of India’s Standard Treatment Workflows 2022 (stw.icmr.org.in), recommends absolute indications for cholecystectomy in asymptomatic cholelithiasis with suspected malignancy, calculi greater than 2.5-3 cm, solitary polyp larger than 1 cm, multiple calculi, porcelain (calcified wall) gallbladder, chronic hemolytic anemia, transplant recipient and children. Literature adds to this list anomalous pancreatic–biliary anatomy including a long common channel of bile and pancreatic ducts, choledochal cysts, adenomas, choledocholithiasis, bariatric surgery, diabetes, residence with poor accessibility to urgent healthcare delivery and those on immunosuppressant therapy.
There is a thus a need for risk stratification to selectively manage those in high-risk groups with asymptomatic cholelithiasis given that modern surgery techniques have low morbidity risks. High risk patients if asymptomatic, should be advised surgery.
Ramya S and Sanjiv Lewin
St. John’s Medical College and Hospital
Bangalore 560034
Karnataka
sanjiv.lewin@stjohns.in
Recommended reading
Lee BJH, Yap QV, Low JK, Chan YH, Shelat VG. Cholecystectomy for asymptomatic gallstones: Markov decision tree analysis. World J Clin Cases 2022; 10(29): 10399-10412
Goswami AG, Basu S. Cracking the silent gallstone code: Wait or operate? World J Clin Cases 2024; 12(16): 2692-2697 Illige M, Meyer A, Kovach F. Surgical Treatment for Asymptomatic Cholelithiasis Amer Fam Phys 2014; 89(6): 468-470.
GurusamyKS, SamrajK. Cholecystectomy for patients with silent gallstones. Cochrane Database of Systematic Reviews 2007, Issue 1. Art. No.: CD006230. DOI: 10.1002/14651858.CD006230.pub2.
Indian Council of Medical Research and Ministry of Health and Family Welfare, Government of India. Gallstone Disease. Standard Treatment Workflows for India. 2022; 3: 39.
A Rare Case of Acute Deep Vein Thrombosis Following Conservative Management of Achilles Tendon Rupture: A Case Report
Abstract Achilles tendon injuries are prevalent among physically active individuals, especially middle-aged athletes. Conservative management involving immobilization is commonly employed for near-total ruptures; however, it predisposes patients to complications like deep vein thrombosis (DVT). This report presents a case of a 56-year-old male who developed acute DVT within seven days of using a pneumatic walker boot for a near-total Achilles tendon rupture sustained during sports activity. The case highlights the paradigm shift in the management of Achilles tendon injuries and DVT, emphasizing early mobilization and the use of direct oral anticoagulants (DOACs). Potential reasons for early DVT onset and preventive strategies are also discussed.
Keywords: Achilles tendon rupture, deep vein thrombosis, conservative management, anticoagulation, pneumatic walker boot.

Figure 17 DVT
Introduction
Achilles tendon ruptures are a common injury, especially among middle-aged individuals engaging in sports activities. Conservative management, typically involving immobilization, is a widely accepted treatment approach for partial or near-total tendon ruptures. However, prolonged immobilization increases the risk of venous thromboembolism (VTE), including deep vein thrombosis (DVT) and pulmonary embolism (PE) (1). Advances in DVT management emphasize the importance of early diagnosis and therapeutic intervention to prevent life-threatening complications (2). This report highlights a case of acute DVT following conservative management of an Achilles tendon rupture and discusses the implications of evolving therapeutic protocols.
Case Presentation
Patient History and Clinical Presentation
A 56-year-old male with no prior medical history sustained a sports-related injury while playing badminton. The patient presented with pain, swelling below the left ankle, and an inability to bear weight on the affected side. Clinical examination revealed tenderness and a palpable gap along the Achilles tendon, suggestive of rupture. Initial management included ice application, non-steroidal anti-inflammatory drugs (NSAIDs), and immobilization.
Diagnostic Workup and Initial Management
An MRI confirmed a near-total rupture (90%) of the left Achilles tendon. The case was referred to an orthopedic surgeon, who recommended conservative management with immobilization. A pneumatic walker boot with an air cast and wedge for plantar flexion was applied, allowing limited movement. The patient was advised periodic follow-up for reducing the height of the plantar flexion wedge.
Complications and Diagnosis of DVT
By the eighth day of immobilization, the patient reported mild calf swelling and cramping pain. A venous Doppler ultrasound identified acute DVT involving the popliteal and calf veins. Blood work revealed elevated D-dimer levels but no evidence of thrombophilia or malignancy.
Management and Outcome
Anticoagulation therapy was initiated with low molecular weight heparin (LMWH, Enoxaparin 40 mg subcutaneously) and transitioned to oral Rivaroxaban (15 mg twice daily for three weeks, followed by 20 mg once daily for three months). Compressive stockings were recommended, and early mobilization was encouraged. The patient’s symptoms resolved gradually without further complications. Follow-up imaging confirmed thrombus resolution.
Discussion
DVT Risk in Immobilized Patients
Immobilization of the lower limb is a well-recognized risk factor for DVT due to reduced venous return and stasis. Achilles tendon rupture significantly increases the risk of early onset DVT, as it impairs calf muscle function and reduces venous return from the lower limb. Although this patient had limited mobility with a pneumatic walker boot, prolonged plantar flexion and reduced calf muscle activity likely contributed to venous stasis and thrombus formation (3, 4).
Potential Mechanisms of Early-Onset DVT
- Mechanical Factors: Prolonged immobilization impairs calf muscle pump function, causing venous pooling.
- Inflammatory Response: Tissue injury and repair processes may trigger a hypercoagulable state (5).
- Postural Considerations: Plantar flexion exacerbates venous stasis by altering venous flow dynamics.
Paradigm Shift in DVT Management
Traditional DVT management relied on immobilization and unfractionated heparin. Current protocols emphasize early mobilization, prevention strategies, and direct oral anticoagulants (DOACs) like Rivaroxaban, which offer convenient dosing and fewer monitoring requirements compared to Warfarin. Prophylactic anticoagulation in high-risk immobilized patients is increasingly being adopted to mitigate VTE risks.
Advances in DVT Management
- Direct Oral Anticoagulants (DOACs): DOACs such as Rivaroxaban and Apixaban have become first-line treatments for DVT due to their efficacy, predictable pharmacokinetics, and ease of administration (6).
- Early Mobilization: Encouraging early weight-bearing and physical activity reduces the risk of post-thrombotic syndrome and recurrent VTE (7).
- Prophylaxis in High-Risk Patients: In cases of immobilization, prophylactic anticoagulation with LMWH or DOACs may be warranted (8).
Preventive Strategies
- Patient Education: Early recognition of DVT symptoms, such as calf swelling and pain, is critical.
- Thromboprophylaxis: Prophylactic anticoagulation should be considered in immobilized patients with additional risk factors, such as obesity or prior VTE (9).
- Mechanical Prophylaxis: Compression stockings and intermittent pneumatic compression devices may reduce venous stasis (10).
Implications for Clinical Practice
The case underscores the importance of balancing immobilization with early mobilization in the management of Achilles tendon injuries. Incorporating patient-centered care, risk stratification tools, and evidence-based prophylactic measures can enhance outcomes and minimize complications.
Conclusion
This case underscores the need for heightened vigilance for DVT in patients undergoing immobilization for Achilles tendon injuries. Prophylactic strategies, including early mobilization and anticoagulation, should be considered, especially in high-risk cases. Advances in anticoagulation therapy, particularly the use of DOACs, have significantly improved the safety and convenience of DVT management. Clinicians should maintain a high index of suspicion for VTE in immobilized patients and adopt preventive strategies to optimize outcomes.
Col(Dr) Mohan Kubendra
References
- Healy, B., & White, B. (2020). Deep vein thrombosis and pulmonary embolism: Current treatment and future prospects. British Medical Journal, 369, m2395. https://doi.org/10.1136/bmj.m2395
- Patel, M. R., et al. (2011). Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. New England Journal of Medicine, 365(10), 883-891. https://doi.org/10.1056/NEJMoa1009638
- Turetz, M., et al. (2018). Epidemiology and pathophysiology of pulmonary embolism. Seminars in Interventional Radiology, 35(2), 92-98. https://doi.org/10.1055/s-0038-1642036
- Willits, K., et al. (2016). Operative versus nonoperative management of acute Achilles tendon ruptures. American Journal of Sports Medicine, 44(8), 2126-2132. https://doi.org/10.1177/0363546515626428
- Kakkos, S. K., et al. (2021). European guidelines on chronic venous disorders. European Journal of Vascular and Endovascular Surgery, 61(1), 9-82. https://doi.org/10.1016/j.ejvs.2020.09.023
- Bauersachs, R., et al. (2010). Oral rivaroxaban for symptomatic venous thromboembolism. New England Journal of Medicine, 363(26), 2499-2510. https://doi.org/10.1056/NEJMoa1007903
- Guss, D., & Rosenwasser, M. (2017). Improving outcomes in Achilles tendon repair. Journal of the American Academy of Orthopaedic Surgeons
Rat mite bite causing urticaria like rash
Extract
Mrs. A.R, a lay person reported feeling of insects crawling all over her body. She investigated and found out that it is due to rat mite bites. Rat mite bites causing urticaria like rash should go into differential diagnosis of itchy lesions of the skin.
Case report
On 1/3/21, at night, she felt crawling sensation all over her body with itching and next morning she saw red elevated rashes on her, chest, abdomen, and legs. She noticed small black insects on her bed covers and, on her phone. She contacted Dr B who advised her to wash all the clothing and sheets daily and take Avil. He also told her the insects must be coming from her terrace garden.
Mrs. A.R did as advised, but the invasion continued, and an internet search revealed the creature had a close resemblance to rat mite. There was no doubt at all as to the identification that it is indeed rat mite.
But how did it colonize in her garden? A bit more of detective work found rats coming up the drainpipe to her apartment terrace and she found evidence of these nibbling the shoots of her plants and any number of these mites were found.
Preventive action in the form of anti-rodent measures and insecticide sprays have helped to prevent recurrence and her plants too are in better shape.

Figure 18 Urticarial Rashes
Discussion
Mite bite can cause many illnesses. Fortunately rat mite does not cause any systemic illness except the bite induced local reaction which is self-limiting and fades away in 2 weeks’ time. Rodents are omnivorous and eat the tender shoots of plants and in her case, she first noticed the destruction caused to her Tulasi plant. Normally when we discuss differential diagnosis of itchy rash, we do not think of rat mite bite. Literature search did not reveal many reports from our country. Keeping in mind, that rodent infestation is very common in our country, it is suggested, that when one sees an itchy rash, it is better to exclude rat mite bite as a likely cause.
Conclusion
A case of rat mite bite induced itchy rash is reported. This possibility is to be kept in mind when ever a patient reports crawling sensations associated with itchy rash, it is worth looking for this mite in the immediacy of the person.
Mrs. Aarthi Ranganath
DR. S. B. Swathy
An unusual presentation of Psoriatic Arthropathy
An unusual presentation of Psoriatic arthropathy
A 50-year-old man reported with a history of pain in his back shoulders and hip. He said these have been there for many years and doctors have given him pain killers and advised some exercises. His X-rays of shoulder and spine show some spondylitic changes. But the movements of the shoulders and hip were possible but painful. His work involved lifting weights and he worked as a professional cook
Examination revealed a well-built man and a general examination was normal His left and right ankle skin showed patches of Psoriasis. A tentative diagnosis of Psoriatic Arthritis was made and he was put on 10mgs Methotrexate once a week with folic acid cover six weeks ago. He came after six weeks and said he was much better and was able to do his work without taking any painkiller. He was asked to continue and come for review after another six weeks.
Discussion
Normally Psoriatic arthritis affects the small joints od hands and feet. Big joint and spine involvement is rare. In this patient there was involvement of spine, shoulders, and hip without involvement of small joints. Maybe the reason why the diagnosis was missed for so long.
Miscellany
What is new
PIPAC
Pressurized intraperitoneal aerosol chemotherapy, or PIPAC, is a new treatment technique that gives chemotherapy in the form of a pressurized aerosol, or spray, directly into the abdominal cavity. PIPAC is safe, and most people handle it well. It has fewer side effects than regular chemotherapy. Complications....
PIPAC is most often used for end-stage peritoneal carcinomatosis. It may be an option if one has stomach cancer; platinum-resistant, recurrent ovarian cancer (a type that comes back 6 months after treatment with platinum-based chemotherapy); or colorectal cancer, and surgery isn’t an option.
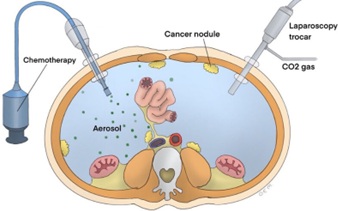
Figure 19 PIPAC
It may also help if tumours in stomach, pancreas, liver, or appendix that have spread to the abdomen.
PIPAC is a simple procedure that takes less than an hour. It is known as a minimally invasive surgery as it involves making small cuts. These are used to place a trocar inside your belly. It will help to guide a camera, or laparoscope, and other surgical tools for the procedure.
During PIPAC, the doctor injects the medication into the belly through a nebulizer, a machine that turns liquid medicine into a fine mist. That helps it go more deeply into the body. Once the drug is inside, 30 minutes wait as it goes to work.
Doctors are studying a new, faster system with a shorter wait time of 2-3 minutes. It may be offered in the future.
While it is still new, PIPAC’s results are promising. In a recent study, more than half the people who had PIPAC reported smaller tumours and relief of symptoms.
We need more research to understand what happens with different tumours. Experts should know more about PIPAC after randomized clinical trials and large studies comparing PIPAC’s results with regular chemotherapy for specific tumours.
Benefits of PIPAC
Improved Efficacy: By directly targeting cancer cells in the abdomen, PIPAC has shown potential for better tumor response rates compared to conventional chemotherapy.
Reduced Side Effects: Since the chemotherapy is confined to the abdomen, patients may experience fewer systemic side effects often associated with traditional chemotherapy. PIPAC is a promising treatment option for patients with peritoneal surface cancers. These are aggressive cancers that have spread to the lining of the abdomen and are often resistant to traditional chemotherapy.
Improved Efficacy: By directly targeting cancer cells in the abdomen, PIPAC has shown potential for better tumor response rates compared to conventional chemotherapy.
Reduced Side Effects: Since the chemotherapy is confined to the abdomen, patients may experience fewer systemic side effects often associated with traditional chemotherapy.
Combination Therapy: PIPAC can be used in conjunction with other treatments, such as surgery, to enhance overall treatment outcomes.
While PIPAC shows promise, it is essential to consult with a qualified medical professional to determine if it is a suitable treatment option for individual patients.
The greater omentum
A vibrant and enigmatic immunologic organ involved in injury and infection resolution.
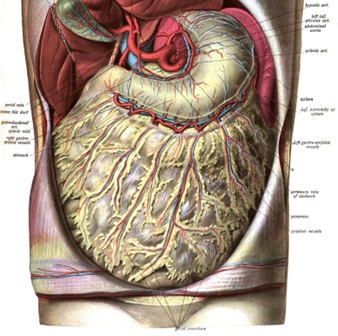
Figure 20 Greater Omentum
Once thought of as an inert fatty tissue present only to provide insulation for the peritoneal cavity, the omentum is currently recognized as a vibrant immunologic organ with a complex structure uniquely suited for defence against pathogens and injury. The omentum is a source of resident inflammatory and stem cells available to participate in the local control of infection, wound healing, and tissue regeneration. It is intimately connected with the systemic vasculature and communicates with the central nervous system and the hypothalamic pituitary adrenal axis. Furthermore, the omentum has the ability to transit the peritoneal cavity and sequester areas of inflammation and injury. It contains functional, immunologic units commonly referred to as “milky spots” that contribute to the organ’s immune response. These milky spots are complex nodules consisting of macrophages and interspersed lymphocytes, which are gateways for the infiltration of inflammatory cells into the peritoneal cavity in response to infection and injury. The omentum contains far greater complexity than is currently conceptualized in clinical practice and investigations directed at unlocking its beneficial potential may reveal new mechanisms underlying its vital functions and the secondary impact of omentectomy for the staging and treatment of a variety of diseases.
In summary, the omentum is an enigmatic immunologic organ uniquely suited for defence against pathogens and injury within the peritoneal cavity. The microscopic functional unit of the organ, the milky spot, is rich in macrophages and lymphocytes organized around a specialized postcapillary venule allowing for the rapid influx of inflammatory mediators into the peritoneal cavity in response to injury and infection. These functional units are widely distributed throughout the adipose-rich regions of the organ and, along with a population of resident stem cells, are largely responsible for the remarkable properties of infection control, wound healing, and tissue regeneration that are widely appreciated and applied clinically. Thus, the omentum is much more than visceral fat and peritoneal insulation. It is a versatile Shock.
Further reading: https://www.ncbi.nlm.nih.gov/books/NBK448192/
Meet the microbiome's 'dance partner': The hidden kingdom of viruses living in your gut
Amber Dance
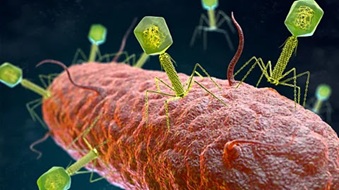
Figure 21
Human innards are teeming with viruses that infect bacteria. What are they up to?
You have probably heard of the microbiome – the hordes of bacteria and other tiny life forms that live in our guts. Well, it turns out those bacteria have viruses that exist in and around them – with important consequences for both them and us.
Meet the phageome.
There are billions, perhaps even trillions of these viruses, known as bacteriophages ("bacteria eaters" in Greek) or just "phages" to their friends, inside the human digestive system. Phageome science has skyrocketed recently, says Breck Duerkop, a bacteriologist at the University of Colorado Anschutz School of Medicine, and researchers are struggling to come to grips with their enormous diversity. Researchers suspect that if physicians could harness or target the right phages, they might be able to improve human health.
"There will turn out to be good phages as well as bad phages," says Paul Bollyky, an infectious disease physician and researcher at Stanford Medicine. But for now, it is still not clear how many phages occupy the gut – perhaps one for each bacterial cell, or even fewer. There are also bacteria that contain phage genes but are not actively producing viruses – the bacteria are just living their lives with phage DNA tagging along in their genomes.
And there are lots of phages still unidentified. Scientists call these the "dark matter" of the phageome. A big part of current phage research is to identify these viruses and their host bacteria. The Gut Phage Database contains more than 140,000 phages, but that is surely an underestimate. "Their variety is just extraordinary," says Colin Hill, a microbiologist at University College Cork in Ireland.
Scientists find phages by sifting through genetic sequences culled from human faecal samples. That is where researchers found the most common gut phage group, called crAssphage. (Named for the "cross-assembly" technique that plucked their genes out of the genetic mishmash.) In a recent study, Hill and colleagues detailed a light-bulb shape for crAssphages, with a 20-sided body and a stalk to inject DNA into host bacteria.
The gut is an ecosystem, like the woods, and phages are bacteria predators, like wolves are deer predators. The gut needs phages like the woods needs wolves.
It is not clear whether crAssphages make a difference to human health, but given that they infect one of the most common groups of gut bacteria, Bacteroides, Hill would not be surprised if they did. Other common groups, which also infect Bacteroides, include the Gubaphage (gut bacteroidales phage) and the LoVEphage (lots of viral genetic elements).
Phageomes vary widely from person to person. They also change depending on age, sex, diet and lifestyle, as Hill and colleagues described in the 2023 Annual Review of Microbiology.
Though phages infect bacteria and sometimes kill them, the relationship is more complicated than that. "We used to think that phage and bacteria are fighting," says Hill, "but now we know that they're actually dancing; they're partners."
Phages can benefit bacteria by bringing in new genes. When a phage particle is assembling inside an infected bacterium, it can sometimes stuff bacterial genes into its protein shell along with its own genetic material. Later, it squirts those genes into a new host, and those accidentally transferred genes could be helpful, says Duerkop. They might provide resistance to antibiotics or the ability to digest a new substance.

Figure 22
Phages keep bacterial populations fit by constantly nipping at their heels, says Hill. Bacteroides bacteria can display up to a dozen types of sugary coats on their outer surfaces. Different coats have different advantages: to evade the immune system, say, or to occupy a different corner of the digestive system. But when crAssphages are around, Hill says, the Bacteroides must constantly change coats to evade the phages that recognize one coat or another. The result: at any given time, there are Bacteroides with different coat types present, enabling the population as a whole to occupy a variety of niches or handle new challenges.
We each have a unique phageome constantly interacting with our microbiome (Credit: Getty Images)
Phages also keep bacterial populations from getting out of hand. The gut is an ecosystem, like the woods, and phages are bacteria predators, like wolves are deer predators. The gut needs phages like the woods needs wolves. When those predator-prey relationships are altered, disease can result: researchers have observed phageome changes in inflammatory bowel syndrome (IBS), irritable bowel disease and colorectal cancer – the viral ecosystem of someone with IBS is often low in diversity, for example.
People try to re-balance the gut microbiome with diets or, in extreme medical cases, faecal transplants. Tackling phages might provide a more fine-tuned approach, Hill says. As a case in point, scientists are seeking phages that could be used therapeutically to infect the bacteria that cause stomach ulcers.
Perhaps we should be grateful for the trillions of phages managing the gut's ecosystem. Without them, Hill suggests, a few kinds of bacteria might quickly come to dominate – potentially leaving you unable to digest some foods and subject to gas and bloating.
The wild and wondrous phageome is a dance partner for bacteria and humans alike.
Magic Cure
Miscellany
Magic cure
Late Dr. K. S. Hande was a general practitioner like me and like me, has gone through difficult times in the early years of his practice. When patients are few and far between, one has lots of idle time. This time sadly must be spent in the clinic, as one cannot afford to be elsewhere for the fear of losing even that occasional patient.
While my pass time was reading, his was to stand outside his clinic and watch the humanity go by. One day, some 35 years ago, when he was indulging in this favorite pastime, to his surprise he saw one of his patients who had visited him a few days earlier pass by cheerfully waving a greeting.
This patient really had no business to be walking around so cheerfully because when he had visited the doctor, he was a very sick person with X-ray confirmed pneumonia. How then he got so well? Why did he not turn up the next day as advised? Did he go to another doctor and get better? Did I do anything wrong? Was my fee too much that drove this man away from me? These were the worrisome thoughts that Dr. Hande had.
He got the patient to come in and asked him,

Figure 23
‘What had happened, why you did not turn up the next day?’
‘What saar[sir], you gave magic injection that day, next day my fever went, second day my cough went and yesterday I ate well and felt fit and now I am on my way to work. I did not come because your one injection of that magic medicine cured me,’ the patient said. A quick examination revealed complete clearance of his lungs! Dr. Hande had given the patient 400,000 units of procaine penicillin. That was how the drug acted in those days!
One cannot think of such cures now. We have now made a mess of the treatment of infections by indiscriminate use of antibiotics and the germs have developed resistance to most antibiotics and society is paying a heavy price for the physician’s folly! A dreaded time may soon arrive when we see patients dying due to these multidrug resistant infections.
Rashomon Effect
The 40-year-old gentleman was in deep distress. His wife was caressing his left shoulder in a bid to alleviate his pain. Within the last 48 hours, he has met three doctors (specialists to be precise) and underwent an ECG, ECHO, MRIs of shoulder and neck bone, and a battery of blood tests. The wife's hands were overflowing with the prescriptions, bills, and the lab reports. Being an IT professional, he has been suffering from neck pain often. Three days back, the pain started to shift to his left shoulder and arm. Naturally, he googled his symptoms which indicated the possibility of an imminent heart attack. The couple had rushed to a local doctor who performed blood tests and ECG and sent him to a cardiologist.
The cardiologist thought it could still be a myocardial ischemia and performed an echo test and Troponin. It turned out to be normal but to be on the safer side, he prescribed low dose blood thinners, cholesterol medications and advised him to get an orthopedic opinion.
The pain was excruciating and the orthopedician being a specialist in keyhole surgeries suggested that it could be a tear in the shoulder tendons since the patient was a diabetic. He performed an MRI of the shoulder which was equivocal. He gave him some more medications and suggested he meets a neurologist ‘just in case’ it could be a nerve problem. After examination, the neurologist too thought it could be a diabetic or viral neuropathy based on the high diabetes. He advised a few tests and an MRI of the cervical spine. Finally, it turned out to be a slipped disc in the neck bone and he landed in our net.
What we see here is a common healthcare situation of late. Every specialist sees the patient and his symptoms from his specialized narrow perspective. The clinical notes, investigations and management are tailored to the doctor's specialization. This is what I would state as Rashomon Effect.
Rashomon was a famous movie directed by the celebrated Japanese auteur, Akira Kurosawa. In this movie, a murder scene is described by the different witnesses in their own point of view. All their views are different from one another. But they all believed that they are speaking the truth because it is their own correct perspective.
Similarly, every medical specialist has their own approach towards the patient, typically focused on the system in which they have specialized. Upper stomach pain is seen as esophagitis by a gastroenterologist, angina by a cardiologist and costochondritis by the orthopaedician. If we look at their clinical notes and examination findings, it would match their diagnosis since their mind is blinkered. The specialized mind fills the gaps with his previous observations, knowledge about their organ system and myopic training.
With increasing super specialization, the patient is not seen as a whole but an affected organ system. The specialist of the organ system falls prey to the Rashomon effect and explains the patient's symptoms from his perspective. It is difficult to avoid this in the upcoming future since general practitioners are on the wane now. Unless the medical community talks about this, this could reach tremendously dangerous propositions.
[Source not clear as it came as a forwarded message to me]
